Enough is enough: 'junior' is not the word
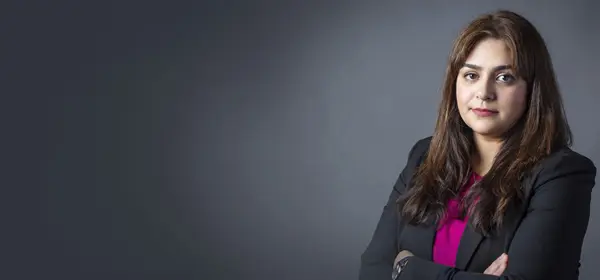
As the BMA campaign for pay restoration gathers pace, The Doctor has spoken to a range of junior doctors about why they are considering industrial action ahead of a ballot expected in early January. In the fourth of a series of interviews, Ben Ireland speaks to Barnsley doctor Ellen Newberry
‘Every job comes with its hardships, but people don’t realise that one doctor might be covering six, eight or even 10 wards overnight – which could be 200 to 300 patients out of hours.
‘We’re being run ragged between wards and F1s are getting £14 an hour for the privilege. It’s not a huge amount better the further up you go. We don’t get paid as much as people think we do.’
The crux to the BMA junior doctors committee proposed industrial action for Ellen Newberry, a medical registrar at Barnsley Hospital NHS Foundation Trust who worked at Sheffield Teaching Hospitals NHS Foundation Trust for her three-year IMT (internal medicine training) programme, is that doctors carry a very senior level of responsibility despite being classed juniors.
‘I hate the phrase junior doctor. Sometimes members of the public assume it means a medical student. I’m in my 7th year of medical work now and there are people 15 years into their careers still called "junior" doctors.
'Overnight someone at my stage is often the most senior doctor in the hospital, so when people dismiss us as "junior" it’s quite galling, because it’s a lot of responsibility. F1s are brand new doctors, but they too have a lot of responsibility. It’s infantilising.’
She doesn’t like to compare doctors’ income to that of other professions but makes the point that junior doctors are making life and death decisions for relatively little pay while many people believe they’re earning six-figure salaries.
NHS pay
Dr Newberry believes all NHS staff are underpaid, not just doctors. She worked as an HCA (healthcare assistant) between 2007 and 2011, before embarking on five years of medical school and taking on £45,000 in student debt. As a HCA, she earned a little less than today’s foundation year 1 doctors do, and that’s without taking inflation into account.
And since her own F1 year in 2016, she says: ‘My job has got significantly harder. I don’t mean in terms of the extra responsibility – I find that part enjoyable and stimulating – I mean sheer volume. And I know my pay package has gone down significantly [in real-terms] in that period.’
For Dr Newberry, ‘the biggest challenge is the medical take’. A take shift often starts with 20 to 30 patients waiting to be seen having been admitted by the emergency department.
‘They could be waiting for hours and hours,’ she says. ‘The difference between when I started is that now it’s relentless, not just a terrible few weeks or months over winter. When I started, there at least tended to be occasional quieter periods where you might get on top of the admission list.’
And she says it’s ‘not uncommon’ for F1s on the wards to be looking after more patients than the Royal College of Physicians deems appropriate for their level of experience.
‘That’s before you factor in medical outliers; when 30 patients between three junior doctors might become 50.’
Pay erosion has led to ‘swathes’ of junior doctors moving overseas, ‘because we’re not paying as well’, and this leads to a ‘vicious cycle’ whereby rotas have gaps, exhausted doctors push themselves to fill them on their days off because they don’t want colleagues to suffer, sometimes clocking up 70-hour weeks, while trusts are forced to ‘fork out for locums’ to cover and training places are depleted.
People are beginning to realise how much they have lost and are starting to get angry
Dr Newberry
Dr Newberry’s point is not that doctors are poor compared with the average worker, but that they went into their careers thinking they would have well-paid jobs in return for their hard work and dedication.
‘It’s a difficult topic to broach, but many doctors now struggle to get on the property ladder whereas public perceptions are that that’s something doctors can afford.
'It used to be something that an F1 might be able to contemplate. Now, I don’t know a single F1 anywhere near that position.’
By the BMA’s calculations, junior doctor pay has eroded in real terms by 26 per cent since 2008, though Dr Newberry says different methods put that at 30%.
‘If we don’t do anything – it’s not going to stop here,’ she says.
‘If you don’t draw a line now, where do you draw it? People are beginning to realise how much they have lost and are starting to get understandably angry about it.’
- Until September 2024, resident doctors were referred to as ‘junior doctors’ by the BMA. Articles written prior to this date reflect the terminology then in use