Enough is enough: junior doctors' fight for fairness
As the BMA campaign for pay restoration gathers pace, The Doctor has spoken to a range of junior doctors about why they are considering industrial action ahead of a ballot expected in early January. In the first of a series of interviews, Ben Ireland speaks to specialty trainee 2 Priyesh Parekh
There's a fable which says that if you put a frog in boiling water it will jump out, but if you put it in cold water and slowly increase the temperature, it won't notice and will slowly boil to its death.
'Junior doctors feel like that frog in the cold water,’ says Priyesh Parekh, a specialty trainee 2 in paediatrics working at University Hospitals Coventry and Warwickshire NHS Trust.
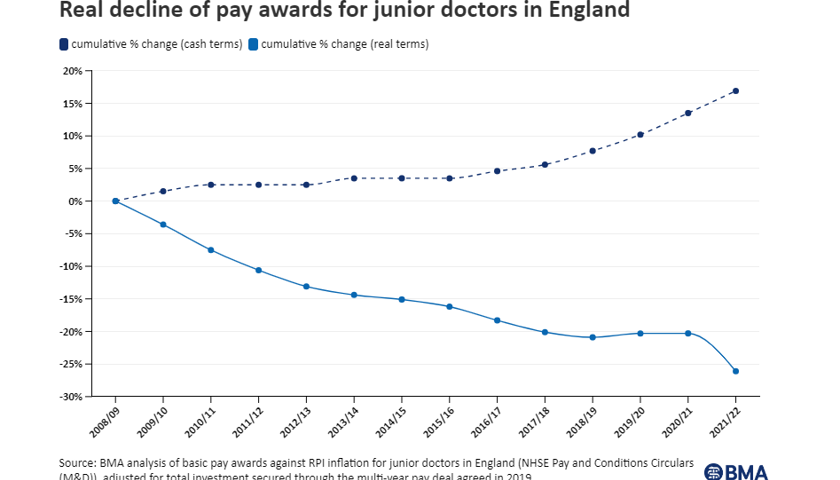
'We cannot continue like this after more than a decade of below-inflation pay awards coupled with poor retention has led to junior doctors doing more for less.'
Dr Parekh feels that the good will, this desire to work in a profession that is intrinsically caring, the years of hard work it takes to get there, not to mention the amount of student debt taken on to fund study, has long been taken advantage of by the Government when deciding on junior doctors' pay.
On a hospital rotation in his third year of medical school, he recalls one doctor saying 'you should leave medicine'.
'I remember dismissing it instantly because I had worked so hard to get there,' he says. 'Sometimes I think back to that moment. When you see it for yourself and know the issues you realise why.'
Dr Parekh has seen colleagues move into careers such as management consulting and notes how firms are targeting highly skilled medical professionals they can snap up. He joined one webinar to learn more and was 'amazed' to find 200 other doctors had also logged in.
And 'it's medical students too', he says. 'They have seen what it’s like and don't even want to give it a year.'
He says: 'I've definitely had moments where I question if continuing in medicine is the right choice.'
And when he looks around and sees overworked consultants being taxed excessively on their pensions, or GPs slogging through five days of 12-hour shifts, the exit door looks appealing.
'A lot of doctors are realising we are being taken for a ride and we shouldn’t accept it – and it’s not looking rosy at the top either,' he says.
'We're sometimes a soft profession because we think about how it looks on us, so it’s hard for us to find our voice [but] there's definitely a need for change.'
Ultimately, Dr Parekh comes back to the reason he chose medicine in the first place: 'When you actually treat the patients, it’s a really rewarding career. If you can solve a patient's problem, applying knowledge you've learnt, it's really nice.
'Being a doctor is great when you can do the doctoring – but when you're constantly focusing on other stuff, like writing consultants' notes, you're basically a secretary. In one day of work you've written the equivalent of a novel. But they haven't got anyone else to do it.
'I love those moments but in reality it's only 20 per cent of the time. People put up with it because they hope it will get better and you will start to make those decisions and it’ll be more rewarding.'
After 14 years of pay cuts, we just want to return to what it was
Dr Parekh
But 'all the other things', such as shift patterns, working conditions, pay erosion and car-parking charges ‘makes it a bit more difficult'.
'You want to do something that helps people and that you're proud of, but you want some sort of remuneration,' he adds. 'If you don't properly remunerate people, it devalues them.'
And, after 14 years of real-terms pay cuts, he points out: 'We're not asking for a pay rise, we’re asking for pay to go back to where it was.'
Specialisation disrupted
Junior doctors have also had their progression affected by the COVID pandemic. During the second wave, Dr Parekh was pulled into the 'chaos' of ICU from the ENT rotation he was enjoying and considering specialising in – working up to 76-hour weeks – and missed a respiratory rotation.
Being a foundation year 1 during the pandemic, and moving out of his parents' home, meant 'I found it more acceptable to be doing weekends and nights because social interactions were limited because of COVID.’
However, he says: 'Nowadays it's a lot more difficult because more is going on.'
Rotas are still 'very packed', and people 'put up with' working beyond their hours and taking breaks 'when you can' – including nights and weekends, though 'it’s not comfortable'.
This moment is massive for doctors and, while there is a lot of optimism, if it falls through it would be tragic
Dr Parekh
'The culture is putting up with it among junior doctors,' he says, but notes recent optimism with the success of strikes in other professions such as the Criminal Bar Association, which negotiated a 15% uplift.
'It's always playing on my mind whether staying in medicine is the right thing,' he says.
'Pay restoration would show we are valued. This moment is massive for doctors and, while there is a lot of optimism, if it falls through it would be tragic.'
- Until September 2024, resident doctors were referred to as ‘junior doctors’ by the BMA. Articles written prior to this date reflect the terminology then in use