NHS on the cusp of collapse
NHS on the cusp of collapse
Overcrowding and underfunding have left patients and doctors at risk and, as a demanding summer turns into a winter of alarming challenges, how will the NHS cope? Peter Blackburn talks to doctors across the UK struggling on the front line.
Overcrowding and underfunding have left patients and doctors at risk and, as a demanding summer turns into a winter of alarming challenges, how will the NHS cope? Peter Blackburn talks to doctors across the UK struggling on the front line
‘When I left my shift at 2am there were 56 patients in the majors department – in a space with just 16 bays. Each bay was split in half for two patients and we had to leave one bay free to be used for toileting and another as a drinks station owing to the sheer amount of people in the corridor.
‘It is a terrifying situation.’
Previous experience would suggest this south-west specialty trainee in emergency medicine, speaking to The Doctor anonymously, would be describing a hospital trust at the height of winter – with a flu epidemic and inclement weather driving rocketing demand in accident and emergency departments. But this is a mild autumn day, not a winter war zone.
‘I worked in finance during the 2008 crash before I came into medicine and what we are seeing now is not that dissimilar a story really, it’s all chaos. When you stop to think about winter pressures and how demand is going to go in the next three months, I just don’t know what to think. It is not safe – I can hardly bear to think about it.’
Collective concern
It is a picture playing out in hospital trusts across the country.
One Midlands emergency medicine consultant tells The Doctor the summer was ‘absolutely brutal’.
He says: ‘It felt like winter from five or six years ago. It was just incredibly hard going. We spent the summer with our patients in the corridor with very little space in the hospital and hitting October it felt like January of 2017 or 2018.
‘It is just horrible out there and it is incredibly difficult for people to do their jobs well.’
This is a three-fold crisis: this country’s most beloved national institution is bursting at the seams, patients are suffering and frontline staff have little more to give.
The consultant adds: ‘It’s really corrosive for staff because they are coming into work with patients lining the corridor – we have been putting patients in bits of corridor we have never used before – we are actually expanding into new areas. There have been cardiac arrests on the corridor in a number of places.
‘We are completely under the cosh and I don’t think there’s an emergency department in England or Wales that thinks that patient care isn’t going to suffer over winter. The truth is that it’s already suffering – and it’s not through lack of effort on the part of trusts. Trusts are doing all that they can do, they are engaged in the process of trying to free up beds but it feels a bit like the bottom has fallen out of the system – particularly social care.’
A Sussex nurse adds: ‘We don’t really have a time when we aren’t full to bursting point and are normally on black alert – where the need for beds is just overwhelming.’
But why was the summer so bad – and what might it tell us about the winter ahead?
During the three summer months the NHS averaged 17,536 emergency admissions per day – a 3.6 per cent increase from 2018. Emergency admissions place a huge strain on resources as trusts can’t plan for them and a small increase can cause significant blockages in hospitals. On top of that attendances at emergency departments across England increased by 5.7 per cent and the NHS seems to have suffered a winter hangover, with four consecutive winters of at least 150,000 trolley waits leaving trusts on the back foot heading into spring, summer and autumn.
Consultant's despair
The problems have been exacerbated by the pensions crisis – with consultants being prevented from picking up shifts for fear of dramatically increasing their tax bills. A recent Royal College of Emergency Medicine survey reveals that nearly 90 per cent of consultants who responded said the rules would affect rota gaps at senior levels.
The pressure on NHS hospitals this summer carries a very significant health warning for the NHS this winter. This summer the NHS’s recovery was smaller than in any year since 2011, bar one – 2014, a year which saw an unprecedented fall in four-hour wait performance, dropping 5.4 percentage points between December 2013 and December 2014.
Documents released by trust boards from hospitals around the country do not make for pretty reading. Several documents reference anxiety of staff looking ahead to winter, many raise concerns about the Australian flu season being the worst on record, one East Midlands trust is converting office space for beds and many trusts are launching new systems and pathways to try and cope with demand. In response the NHS has launched its biggest ever winter vaccinations programme and individual trusts are putting new practices in place across their hospitals.
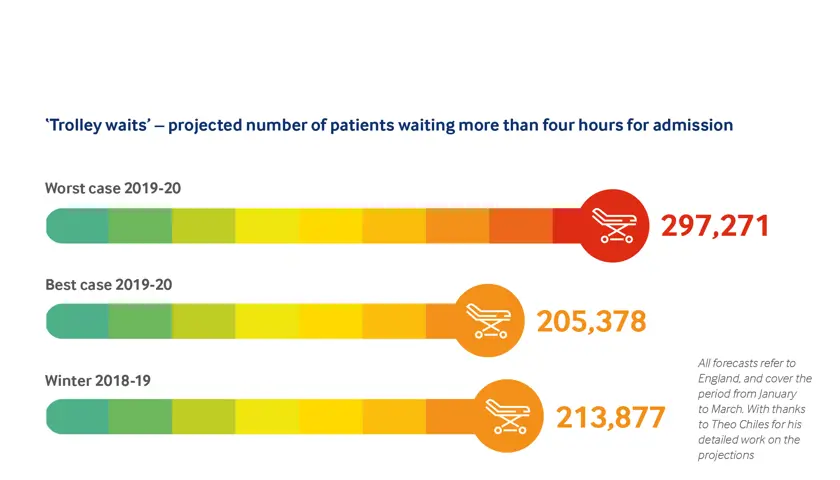
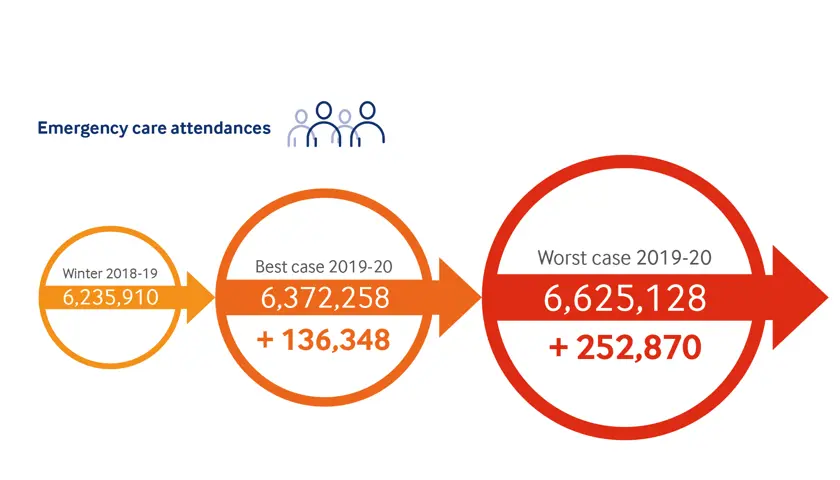
Using national performance data and analysing trends the BMA has made projections for trolley waits, the four-hour wait and attendances and admissions this winter. The projections, which assume that recent trends continue and do not take any future interventions into account, do not make for pleasant reading.
Best-case and worst-case scenarios would represent the most pressurised winter on record. The worst-case scenarios see performance drop markedly: trolley waits rocketing by tens of thousands, attendances and admissions increasing dramatically and four-hour targets likely to drop significantly.
One Midlands emergency department consultant says: ‘It is absolutely daunting looking ahead to winter. I’m not a naturally negative person, I tend to believe we can manage but we didn’t a couple of years ago and we are in a worse place than we were then. There is genuine concern among colleagues about what this particular winter holds and if we have the flu or a lack of medications through Brexit or a lack of people in care homes to look after patients then we are in serious trouble.
‘Emergency departments are the place with the light outside the door that never goes off, but that is playing out in a way that isn’t good for patients and that light can’t stay on forever. Patient care and staff mental health are going to take a real hit if we don’t improve this situation.’
London emergency department consultant Barbara Cleaver tells The Doctor that her trust is doing everything it can to put plans in place, and that wider systems are now recognising these issues are beyond the control of emergency departments, but that she anticipates a ‘difficult winter’.
She says: ‘None of us like to work in an overcrowded department – there is really good evidence that patients get a much worse outcome than if they came in and it wasn’t overcrowded. It’s difficult if you are a kind human being to think that is acceptable. It’s upsetting to come to work and not deliver the care you would like to be delivering because you are overcrowded.’
Dr Cleaver says she is particularly concerned about homeless patients and patients with mental health issues this winter, with demand likely to soar and fewer resources available for appropriate treatment and support across the system.
Staff suffer
Doctors seem to be unanimous in accepting the horror of working conditions, and the expected decline in winter, are affecting patient care – ‘working conditions are actually dangerous and patients may come to harm’, one emergency department consultant says – but the health of staff is a genuine concern, too.
While trusts and NHS leaders might like to talk about resilience of staff during conferences and high-level meetings, the truth is that such consistent pressures take a toll on very many of them.
As the south-west specialty trainee says: ‘When people ask me what training programme I am on and I tell them, they suck through their teeth and they don’t envy me at all. Anyone who comes into any emergency department would wonder why on earth you would go into it because you are asking to be burned out in that environment.’
He adds: ‘It is just not feasible for someone to work that hard for that long in a system at breaking point. The buzzword of resilience is great, but you don’t get through medical school and training without being a resilient individual. It is down to the system.’
The pensions crisis also represents a serious concern ahead of winter. Last month, NHS Providers, which represents hospital, mental health, community and ambulance services, said patients would be at risk of unsafe care unless an ‘urgent solution’ to the problem – which is seeing consultants avoid working extra shifts due to being hit with massive tax bills – is found.
With doctors already on the brink of burnout and the most pressurised winter in history on the horizon can anything be done to avert disaster?
The first answer is yes – with genuine political will and proper investment. The BMA has long campaigned for the NHS to increase its bed stock, and it is crucial this is done before winter begins.
Beds needed
BMA emergency medicine lead Simon Walsh says: ‘Last year the BMA called for a minimum of 10,000 additional hospital beds to be opened across the UK after an analysis of recent years’ performance and hospital occupancy left no doubt that there are insufficient beds to cope with the number of emergency admissions that are required over the winter months.
‘It is notable that even the chief executive of NHS England, Simon Stevens, has recently acknowledged that we need to go into winter with more hospital beds than last year. The problem of course is that trusts don’t have the funding or staff to do that so what is required is for the Government to acknowledge the scale of the problem and to fund these additional beds and staff before it’s too late.’
And steps also must be taken to ensure doctors are not prevented from working by the pensions debacle.
Dr Walsh says there needs to be an immediate increase in funding to health and social care, and also a plan which can better meet the needs of an ageing population.
‘It is going to be too late to wait – the Government needs to take urgent action now before the worst of this winter fully arrives and we face a perfect storm undoubtedly resulting in the worst ever winter on record. I’m afraid the staff cannot bend any more to absorb the pressure of this broken system – I fear for the consequences this winter if action is not taken immediately.’
- Until September 2024, resident doctors were referred to as ‘junior doctors’ by the BMA. Articles written prior to this date reflect the terminology then in use