BMA sets out landmark guidance on physician associates
‘Make no mistake. The current situation on the ground is a failure that today’s publication seeks to address.’
This was the sober and uncompromising assessment delivered by BMA council chair Philip Banfield to assembled members of the press, as the BMA launched its landmark national guidance on how MAPs (medical associate professionals) should be safely utilised within the NHS.
The guidance, which was unveiled during a press conference on 7 March, is the first framework devised by doctors which provides a safe scope of practice for MAPs, a term which encompasses physician and anaesthesia associates.
Setting out six general principles governing the deployment of MAPs, the guidance also uses a simple traffic light-style system determining which procedures, from a by-no-means exhaustive list, should and should not be tasked to such staff.
Among the red lines in the guidance is an absolute prohibition on MAPs being responsible for undifferentiated patients, and a requirement for close supervision when caring for triaged patients.
‘MAPs have an important role in the NHS, but only if we can provide a framework for safe and effective practice,’ Dr Banfield explained.
‘The public does not understand that physician associates work as doctors’ assistants, or that they have increasingly been placed in positions with inadequate supervision and with huge local variation in what they are expected to do.
‘This is a crucial guide for safe practice, drawing on doctors’ expertise and experiences. It is a clear explanation of how MAPs can be employed to maintain the provision of high-quality safe patient care in the NHS.’
The role of MAPs within the NHS is one that has garnered increasing controversy and concern in recent years, owing to uncertainty with the level of responsibility and supervision MAPs should receive, and confusion among many patients as to the professional status of these staff.
This lack of clarity was tragically emphasised in 2022 following the death of Emily Chesterton, with Ms Chesterton having been incorrectly diagnosed by a physician associate working at her GP surgery, whom she had believed to be a doctor.
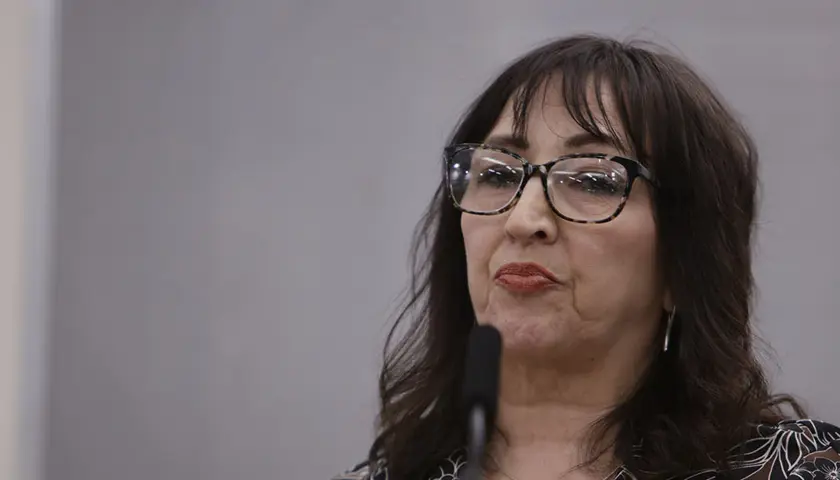
Attending the launch of the guidance, Emily’s parents Marion and Brendan made clear their belief that had such a safety framework been in place two years ago, their daughter would still be alive today.
‘In our daughter Emily’s case, we did not find out she had seen a physician associate on two consecutive occasions and not a GP, until the week before her inquest on 21 March 2023,’ Marion said.
‘We believe that the present title of physician associate is confusing, inaccurate, and sounds grander and superior in qualification and status to a general practitioner and should be changed to “doctor’s assistant”.’
Despite a survey of more than 18,000 doctors revealing that 87 per cent of respondents felt the way in which MAPs are used in the NHS either ‘always’ or ‘sometimes’ posed a risk to patient safety, the Government is pushing ahead with plans to expand the numbers of these staff greatly during the next decade.
Ministers have also succeeded in passing legislation that will see physician and anaesthesia associates being placed under the remit of the GMC, a move the BMA has warned risks further blurring the distinction between doctors and MAPs.
‘We wholeheartedly agree that the Health and Care Professions Council must regulate the use of MAPs and not the GMC,’ warned Marion.
‘If the GMC is the regulator, and there are no plans to set parameters on the scope of practice of MAPs, the confusion and potential risk to patient safety will continue.’