The other, lesser health service
The other, lesser health service
The health service as a whole is under intense pressure, but, in the first part of a new series, and with exclusive data, Peter Blackburn and Ben Ireland examine why the disparity between physical and mental healthcare is so stark.
‘She was bright, kind, caring – and had a real sense of justice and wanting the world to be a fairer place.’ Moira Durdy is remembering her daughter Jess – a talented young engineer who died by suicide aged 27.
Jess had a history of mental health difficulties but kept her struggles to herself. ‘She loved us, and we loved her to bits, but I kind of always had a feeling there was a bit of her that was hidden,’ mum Moira says.
Jess died on 16 October 2020 while at a mental health crisis house in Bristol, having moved in five days before. She was referred there rather than to a scarce psychiatric inpatient unit bed because she was struggling with increasingly intense and intrusive suicidal thoughts.
Jess had previously been prescribed medication in general practice and had a private counsellor. A serious-incident report found failings in her care, including that demand on services had ‘exceeded human capacity to perform all tasks’.
It also found ‘poorly defined’ strategies around escalation of risk and a care system ‘losing clarity under pressure’. It also reported a lack of links between primary and secondary care.
Ms Durdy says Jess felt no one or nothing was helping her and ‘pushed around from one person to another, having to repeat herself all the time and not really getting anywhere’ until she was eventually in absolute crisis.
For Ms Durdy, her daughter’s interactions with health services before her death expose a crisis in mental health services which can now be seen across the country: GPs managing patients too complex for primary care, a lack of communication between primary and secondary care, underfunded specialist services with workforces whose training hasn’t been invested in and insufficient inpatient beds.
Problems are exacerbated in a health landscape in which institutions have been through countless reorganisations and restructures, where reform has infrequently been followed by investment and where oversight and responsibility have been fractured or lost.
The Doctor has spoken to patients and families unable to access specialist support until they are in absolute crisis and often forced to break the bank for private care. Doctors describe a system and workforce stretched to breaking point.
Countless restructures and where oversight and responsibility have been fractured or lost
Royal College of Psychiatrists president-elect Lade Smith likens NHS mental healthcare in 2023 to telling someone with a lump on their breast to ‘come back in three or four years’ time and we will see how you are doing’.
When they return, she says, that patient has stage-four cancer. The Doctor has obtained exclusive data which shows a massive increase in mental health patients presenting at emergency departments in crisis and then trapped there for days or even weeks.
BMA consultants committee mental health lead Andrew Molodynski says the stark statistics show increasing numbers of people are forced into emergency care because of a paucity of specialist services across England.
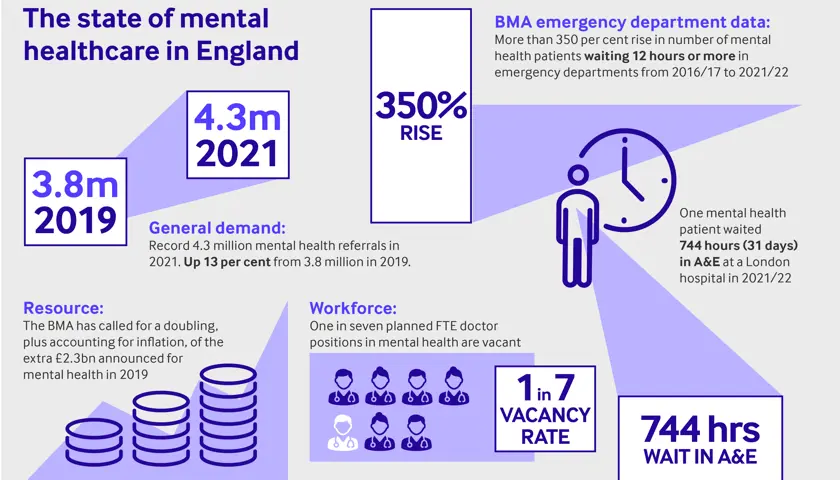
As a result, patients are left in environments which are unfit for purpose and often ‘hugely distressing’. Our data shows the number of mental health patients waiting in acute hospital emergency departments for at least 12 hours more than quadrupled from 2016-17 to 2021-22.
And the figures are still rising. In the space of just seven months from April to October 2022 the numbers had surpassed the annual total from the previous year.
Waiting times soar
In 2016-17, there were at least 1,962 waits of 12 hours or longer at 41 trusts which gave data for that year. In 2021-22 those numbers rocketed to at least 8,971 waits of 12 hours or more at 61 acute hospital trusts.
In the first seven months of 2022-23, there were at least 9,504 at 59 trusts. Many mental health patients spend significantly longer than 12 hours waiting for more appropriate care or assessment. Since April 2016, at least 421 people waited more than 72 hours.
One patient was trapped for 744 hours – 31 days – at a London hospital in 2021-22. The numbers are likely to be much higher as around half of trusts had failed to respond to a freedom of information request at the time of publishing. Experts are united in their damning assessment of this situation.
Cambridge emergency medicine consultant Adrian Boyle tells The Doctor: ‘If you go to a mental health hospital, it’s calm, it’s ordered, it is a recovery environment [whereas] that’s not the environment I work in.’
Dr Boyle, president of the RCEM (Royal College of Emergency Medicine), says patients ‘turn up because alternative access to help is not good’.
Marcus Bicknell, a Nottingham GP with a specialist role in secure mental health and addiction, described the environment at the Queen’s Medical Centre’s emergency department as at times ‘like a World War One casualty station’.
The BMA has also analysed a vast array of NHS datasets to assess the crisis in mental healthcare. Our analysis paints a stark picture of rising demand, a workforce which simply isn’t big enough and funding and resources nowhere near matching the need in communities.
Before the COVID-19 pandemic, rates of mental illness in England had been slowly and steadily rising. The estimation of the prevalence of common mental disorders, conditions such as anxiety or depression, among adults aged 16 to 64 had risen from 18 per cent in 2000 to 19 per cent in 2014. Updated figures are due in 2023-24.
Evidence suggests rates of mental illness may be growing faster among children and young people than adults. Between 2017 and 2022 rates of probable mental disorder increased from around one in eight young people aged seven to 16, to more than one in six.
For those aged 17-19, rates increased from one in 10 to one in four. The numbers of people seeking treatment have risen even more quickly. There are now more than four times as many children and young people in contact with mental health services as there were seven years ago.
Rejected referrals
Mental health services in England received a record 4.3 million referrals during 2021 alone, up from 3.8 million in 2019. Many of these patients aren’t receiving the care they need. Doctors across the country say the number of those referrals being rejected or signposted elsewhere, rather than accepted into secondary care, are rocketing.
Secondary care is overwhelmed by demand and GPs are burdened with managing increased risk and complexity. Hampshire GP partner Emma Nash says demand is increasing and that around a quarter of the circa 100 same-day requests for appointments her practice receives are mental health-related.
Hertfordshire locum GP Neena Jha reports a similar ‘explosion’ in demand. GPs increasingly find their hands tied. Dr Jha says rejected referrals are often accompanied by a suggestion that ‘if it changes or gets any worse then tell the patient to go to A&E’.
Things are similarly difficult in secondary care. One child psychiatrist in the south-west told The Doctor: ‘I’d hate to work in the referrals team. There is a huge increase in the number of referrals, but there are less staff than there were, which can only go in one direction.’
The Doctor spoke to dozens of health professionals about the drivers of these increases. There is an acceptance that reduction in stigma around accessing mental health services is likely to be one reason, but most felt the state of society – where the welfare safety net has fallen away, and society is becoming increasingly unequal – is a major factor.
Dr Molodynski, a consultant psychiatrist in Oxford, adds: ‘Austerity has stripped away a lot of the softer support in society.’ Dr Jha says the effect of this is her patients now often needing mental health care just to ‘cope with life’.
It is clear COVID-19 itself has caused huge damage too – whether through increasing isolation and loneliness, the anguish of long-COVID or the exacerbation of so many existing inequalities in society. Consultant psychiatrist and Dean of the Royal College of Psychiatrists, Subodh Dave, describes an ‘increased psychiatric morbidity’ as a result.
Analysis of NHS data shows the mental health workforce is simply not big enough and that it is not rising at the rate needed to meet demand or the expected increase in demand on services.
For example, the number of people in contact with CAMHS services has increased by 310 per cent since April 2016 while the number of FTE (full-time equivalent) doctors in child and adolescent psychiatry has only risen by 12 per cent in the same time.
On top of this, the average vacancy rate across England for doctors working in NHS mental health services is high, with around one in seven planned FTE roles vacant. Many more are filled with temporary staff.
The average vacancy rate is even higher within nursing roles, at 19 per cent in England, as of last September. One inpatient child psychiatrist working in a tier 4 unit in England told The Doctor their service had a total of five consultant vacancies but that vacancies were ‘constantly’ advertised with ‘no applications’ forthcoming. Continuity of care is often affected, as a result.
Professor Dave describes a ‘vicious cycle’ of poor pay and working conditions which leaves staff taking on more responsibility on wards and in clinics and, ultimately, burning out. He says the Government needs to ‘invest in the wellbeing of the workforce’ urgently.
Dr Smith describes the problem as ‘chronic’ – and says many trusts, with consultant vacancies at 50 per cent, are forced to turn to locum staffing at ‘far greater’ expense, which costs the NHS around £3bn a year.
‘If you’ve got a significant proportion of locums who come in, do the sessions and leave, then leave without helping build and develop the service quality, gradually the quality of the service is not going to improve,’ she says. ‘That’s really concerning.’
Staff in tears
The combination of surging demand and dwindling staff numbers is brutal for staff. One doctor says: ‘It’s impossible to not take it home. You just have this level of exasperation… “I really want to help you, but I can’t”.’
Dr Molodynski adds: ‘The sense of frustration and unhappiness is palpable. We’ve had members of our team in tears at times.’
Funding is a critical issue. While the Government has committed more spending to mental health – at least £2.3bn a year by 2023/24, it says – it is not likely to be anywhere near enough.
In recent years, spending on mental health has increased at a slower rate than overall NHS expenditure and the proportion of the NHS England budget spent on mental health has fallen since 2016/17.
The sense of frustration and unhappiness is palpable. We’ve had members of our team in tears at times
Dr Molodynski
Professor Dave says ‘we’re still playing catch up’ with resource and highlights a lack of beds as an immediate effect of lack of resource. Bed numbers have fallen significantly under successive governments. Learning disability and mental illness beds have seen the largest reduction, of 69 per cent and 23 per cent respectively, since 2010/11.
Professor Dave says: ‘I have been on call when there has been no bed available nationally. There are times when you realise that unless somebody is being detained there’s no hope of finding a bed.’
The effect on patients is brutal. Dr Molodynski says: ‘The more demand there is for the same amount of services means the threshold for accessing services gets higher and higher every year. People who would have been able to access, for example, talking therapy, 15 years ago, in many parts of the country would get nowhere near it these days.’
Two-tier system
Behind every number and every target are thousands of real lives blighted by this crisis. Saskia Homer, a civil servant from Wales, is familiar with the effect under-resourcing has on patients.
Saskia lives with autism, depression and agoraphobia and has attempted to take their own life on ‘numerous’ occasions. Their interactions with mental health services have been torturous – including a three-year waiting list for autism support, another lengthy waiting list for specialised sexual abuse support, a 111 call handler who described them as not sounding ‘very suicidal’ and a ‘frightening’ inpatient stay in a psychiatric hospital.
They also told The Doctor they fear hospitalisation owing to the likelihood of being an inpatient miles away from home in Wales or their parents in Scotland. ‘There’s a disconnect between waiting lists and people’s actual lives.’
Saskia says. ‘The real issue is the waiting times.’ Saskia adds: ‘You don’t feel like you’re going to be helped… You feel like you’re going to be fobbed off from service to service… It makes you lose trust and faith in the mental health system.’
There is a huge increase in the number of referrals, but there are less staff than there were
Child psychiatrist
Doctors are also concerned about the creation of a ‘two-tier’ care system with increasing numbers of people turning to private care for assessment, diagnosis and treatment.
Father-of-two Simon, from the south east of England, felt he had no other alternative when one of his daughters, who was struggling with depression and attending school, was told the waiting list was likely to be years rather than days or weeks.
Simon paid for counselling and an autism diagnosis, which then unlocked other avenues of support, but had to fork out thousands of pounds in savings. Simon says: ‘It must be a dreadful situation to be in where you know that something may be helpful and possibly transformational, but you can’t access it purely because of the cost. I think services need to be far better resourced. People need access to staff like clinical psychiatrists much faster.’
Communities are littered with families such as Simon’s. Reflecting on these stories, the child psychiatrist in an inpatient tier 4 unit says the effects of these delays can be ‘lifelong’.
The BMA is calling on the Westminster Government and NHS England to support mental health services – demanding an expansion of the workforce, ‘robust and frequent’ collection of data, an action plan to attract more clinicians and increased exposure to psychiatric specialties during training.
The threshold for accessing services gets higher and higher every year
Dr Molodynski
The BMA is also urging ministers to protect mental health services against inflation and for a promised £2.3bn increased funding to be brought in line with inflation and then doubled to meet demand.
This investment, it says, must come alongside support for primary care, public mental health, mental health research and estates. Finally, the association is urging an expansion of inpatient mental health beds in England to eliminate inappropriate out-of-area mental health placements.
Appealing for urgent change, Dr Molodynski says: ‘People with mental health problems are enormously varied, but at heart, they have a shared characteristic in that they are in mental health crisis or have mental health problems.
‘If there was any other group of people who had a shared characteristic and we said to this group of people that we’re going to tolerate them having manifestly worse services than other people, tolerate them living on average 15 to 20 years less than the people they live next door to when other factors have been controlled for, we’re going to tolerate them having access rates to evidence-based and NICE guidance-approved services of as low as 20 to 30 per cent, it would be absolutely unthinkable. It would be very clearly a civil rights issue.
‘But for some reason, in this country, and in most countries, we’ve come to a position where we think that’s OK.’ It is abundantly clear, from his testimony and that of other doctors and patients, that it’s not OK.
Additional work by BMA senior policy adviser Olivia Clark and policy advice and research officer Claire Chivers
- Until September 2024, resident doctors were referred to as ‘junior doctors’ by the BMA. Articles written prior to this date reflect the terminology then in use