Symptoms of a crisis
Thousands more people have been detained under the Mental Health Act in recent years. Ben Ireland and Peter Blackburn investigate a healthcare system so ‘broken’ it stores unwell people up until they are in crisis
Tom Burns will always remember the three or four times he ‘got it wrong’.
One of those occasions – among hundreds of ‘painful and distressing’ detentions he has made under the MHA (Mental Health Act) – was a 22-year-old hypomanic art student.
‘I was going to take her in,’ Professor Burns, a retired psychiatrist, recalls. ‘Her dad was desperate for her to stay out, she was desperate to stay out.
‘I let her stay out.
‘She killed herself that night.’
Professor Burns, emeritus professor at the University of Oxford, could hardly give a more powerful example of the seriousness of an assessment under the MHA – of the effect a decision whether to detain or not can have, and the extreme pressure on psychiatrists and other healthcare workers making these choices.
The decisions – ultimately depriving someone of their liberty because they are so unwell and pose a risk to themselves or others – are always a ‘last resort’. Some doctors describe these moments as a ‘privilege’, others as ‘daunting’ and ‘emotionally demanding’. Each is a whirlwind of complexity – with a demanding cocktail of patient history and judgement required from clinicians.
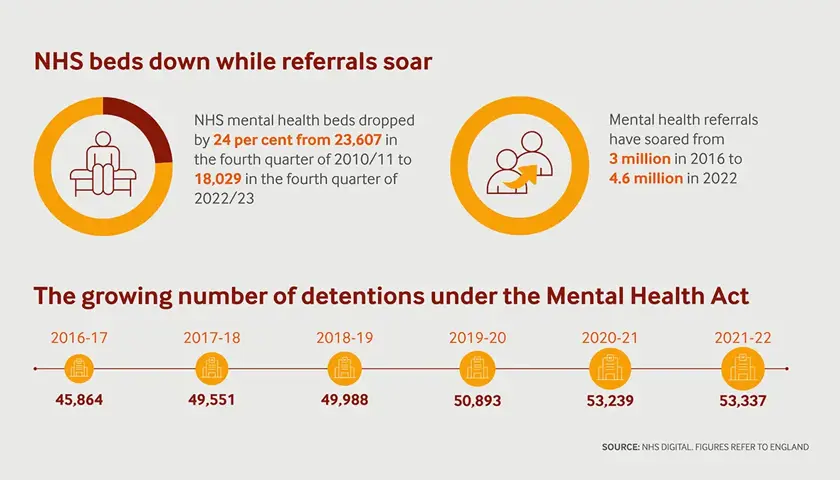
This is the context for an investigation by The Doctor which shows there were thousands more detentions under the MHA in 2021/22 than in 2016/17, with analysis of NHS data highlighting a 16 per cent rise from 45,864 to 53,337, with year-on-year increases.
Through a number of interviews with leading psychiatrists and other healthcare professionals, academics, charities and policy experts, The Doctor has built a picture of the reasons for the rise in seriously ill patients being detained – including the dismantling of the structures that for decades built in continuity of care for mental health patients.
Services overloaded
Doctors reveal the effects of evolving drug misuse, austerity policies crippling deprived communities, and cuts to early intervention services as massive contributing factors.
Psychiatrists also paint a frightening picture of typical inner-city mental health hospitals, with huge rates of severe mental illness among those ‘contained’ on chaotic wards and the rate of acute illness now so high only those with the most worrying conditions are admitted.
On top of this, mental health professionals being under pressure to find beds for those in the most severe crises, leading to many patients being discharged early, piling pressure on stretched community services with police forces now questioning their roles as they face staggering numbers of emergency mental health calls.
It is a ‘perfect storm’ in which seemingly every contributory factor to potential mental ill health has worsened and every part of the system and society – from protection and prevention to treatment – is either buckling under the strain or already long gone.
Prof Burns says a typical ward of 20 patients today might have 18 patients on section. Twenty years ago, he says that would be closer to five. It is, he says, ‘much more overwhelming’ for clinicians.
Sir Robin Murray, professor of psychiatric research at the Institute of Psychiatry at King’s College London, says: ‘In order to get into one of these beds, you have to be very ill.’
He describes crumbling wards ‘full of almost everybody being acutely psychotic’, a ‘very unpleasant’ environment in which patients ‘can interact and make each other worse’.
Swaran Singh, a professor of social psychiatry in Warwickshire, agrees and describes wards as ‘places of containment’ where ‘we provide no care, no compassion’.
The extreme threshold to be admitted to acute wards means there is no space for some patients in severe states of crisis, those who would have been admitted for treatment in years gone by, or they are sent out of area. Psychiatrists also spend more time dealing with court hearings and have less time for hands-on care.
Low bed stock
BMA analysis of NHS data shows the number of NHS mental health beds in England dropped by 24 per cent from 23,607 in the fourth quarter of 2010/11 to 18,029 in the same period of 2022/23.
At the same time occupancy rates have flatlined between 87 and 90 per cent, above the 85 per cent ‘risk threshold’, the level generally considered to be the point beyond which safety and efficiency are at risk.
Meanwhile, mental health referrals have soared from three million in 2016, when comparable records began, to a staggering record 4.6 million in 2022.
Veena Raleigh, an epidemiologist at the King’s Fund, says NHS bed stock has consistently been lower than other comparable countries for years.
In 2021, according to the Organisation for Economic Cooperation and Development, rates stood at 0.34 psychiatric beds per 1,000 people compared to 1.31 in Germany, 2.58 in Japan, and 0.61 in Poland.
‘Services are overstretched,’ she says. ‘And if people don’t have timely access to care, they can get more acutely ill and then come in crisis to the service.’
Dr Raleigh says the ‘supply side issue’ means ‘there are long lead times to access mental health services’.
The system, it seems, is storing up unwell people until they are in absolute crisis.
AMHPs (approved mental health professionals) are responsible for coordinating MHA assessments and detentions with the consultation of doctors. Greater Manchester-based social worker Christina Cheney, chair of the National AMHP Leads Network, reports ‘a pattern of people cycling in and out of hospital’.
She says the lack of beds means ‘people come in too late and are discharged too soon, to make space’ which results in more requests to assess people for detention shortly after they have been discharged from hospital as they ‘very quickly become unwell again’.
As a result, working in acute services becomes ‘ever more pressured’ so recruiting and retaining staff becomes increasingly difficult, and ‘capacity decreases again’ which ‘repeats the impact’.
For patients and staff these horrendous cycles are deeply damaging.
The upshot is more patients than ever being treated by a smaller workforce. Vacancy rates of medical professionals working in mental health services have been above 11 per cent since 2017, and now stand at 15 per cent.
If people don’t have timely access to care, they get more acutely ill and then come in crisis to the service
Dr Raleigh
Admission threshold
Lade Smith, president of the Royal College of Psychiatrists, says often the ‘threshold for coming in is so high that you only get in if you’re detained’.
One statistic perhaps exposes the state of things more powerfully than any other. In 2021/22, 65 per cent (34,838) of detentions took place on admission to hospital, an increase from 56 per cent in 2016/17, while 27 per cent (14,327) took place following admission – a fall from 39 per cent.
It is a stark situation where people are so unwell when they get to hospital that there is no time to see if their condition escalates, or if they can be managed without detention, Dr Smith says.
And Sir Robin, who cares for patients within the National Psychosis Unit at South London and Maudsley NHS Trust, says conditions are so ‘unpleasant’ that people immediately want to leave and are detained when they try.
As a result of pressures in acute wards, problems are pushed back into community services, where staff deal with patients with increasingly severe conditions and, as a consequence, cannot offer therapeutic or preventive services to as many people with milder symptoms. Without early intervention, those patients’ conditions worsen and become severe while others are simply not seen.
Look Ahead, a charity working in East London and Kent, works with patients who have been discharged from hospital. It reports a rising level of acuity among patients amid a wider NHS ‘strategy’ to keep people out of hospital.
Angelina Morgan, the charity’s director of complex specialist services, says hospital bed pressures also mean a growing number of patients being discharged ‘who are not well’ and would previously have stayed in hospital for longer.
This results in some psychotic patients living in the same supported housing as people ‘at other points in their recovery’, increasing pressure on staff.
If a psychiatrist knows you, he or she is much better placed to judge whether you really do need to be in hospital
Prof Murray
'Revolving-door'
A lack of hospital beds hasn’t happened by accident. Successive governments have driven reductions. Alongside this trend, CTOs (community treatment orders) were introduced in 2008 in an apparent bid to reduce the number of so-called ‘revolving-door’ patients and free up those inpatient beds.
They can be applied to people detained under the MHA who are unlikely to pose a risk to others. Use of CTOs peaked in 2020/21, when 6,070 were issued – and 10 per cent (621) of patients were recalled to hospital – but dropped to 5,552 in 2021/22.
However, Prof Burns, who wrote a paper on their use with BMA consultants committee mental health lead Andrew Molodynski, says there is ‘no evidence that they work’.
‘If someone needs to be detained, get them to hospital and treat them,’ he says. ‘To deprive someone of their liberty when they’re well enough to be out of hospital poses an ethical challenge.’
Ms Cheney also wants a rethink on the use of CTOs. She says they have ‘no impact’ on numbers of detentions and suggests they are a back-door mechanism by which ‘compulsory powers are being extended long after an admission is ended’.
Among the most critical factors driving the rise in detentions, psychiatrists say, is the ‘steady decline’ of continuity of care over the last two decades.
‘If a psychiatrist knows you, he or she is much better placed to judge whether you really do need to be in hospital or whether you would manage at home,’ Sir Robin says. ‘Someone seeing you for the first time starts entirely afresh and may be more alarmed than necessary.’
‘If a psychiatrist knows you, he or she is much better placed to judge whether you really do need to be in hospital or whether you would manage at home,’ Sir Robin says.
‘Someone seeing you for the first time starts entirely afresh and may be more alarmed than necessary.’
Dr Smith says the landscape has changed from a model whereby patients would be looked after long-term by the same team, under the overall responsibility of the same consultant – whether they were in hospital or the community.
That meant teams would ‘get to know the patient really well’ and ‘step up support’ when necessary – either seeing them more often or prescribing appropriate medication.
To deprive someone of their liberty when they’re well enough to be out of hospital poses an ethical challenge.
Prof Burns
‘It helped keep people out of hospital,’ says Dr Smith, who practises in South London. ‘And if they did need to come in, you would bring them in earlier, informally. Then when people were in hospital, you could bring them out quicker, knowing you’d be there to watch them.’
Dr Molodynski says: ‘This investigation shows how nearly every mental health patient in hospital is detained now, in what are often not therapeutic, but noisy, busy, austere, and coercive environments.
‘The deinstitutionalisation of the UK over many decades has been a remarkable achievement, but recent reductions in NHS mental health beds have gone too far.
‘People are often discharged much earlier into their recovery because of the lack of beds. Riskier patients are being treated in the community, which is now separated from inpatient care, hindering vital continuity.
‘Increasing pressures mean more staff burn out and conditions only get worse. It’s a vicious cycle and an unsustainable model, as we are increasingly seeing.’
Experts told The Doctor that more patients are presenting in increasingly psychotic states, something that evidence shows is aggravated by drug use – most notably cannabis, which is known to increase the chances of developing psychosis.
Dr Smith says more than 99 per cent of her patients have a co-morbidity of substance use problems, which exacerbates their mental health conditions.
She describes a ‘typical’ situation of an anxious teenager, or often 11 or 12-year-old, growing up in a single parent household on a ‘rough estate’ with a mother working multiple jobs, getting tempted into smoking cannabis by local drug dealers – and slowly developing a habit.
‘It’s no great surprise that when an anxious kid grows their brain in cannabis soup, and happens to have a bit of a family history, that by the time they’re 19 they have their first very full-blown psychotic episode,’ she says.
David Rhinds, a Nottingham-based consultant addiction psychiatrist, says substance misuse services were ‘generally working well’ until austerity and the introduction of the health and social care act in 2012 – when addiction psychiatry was ‘pushed out of the NHS’ resulting in major changes to practice, funding squeezes and less emphasis on addiction as a health issue.
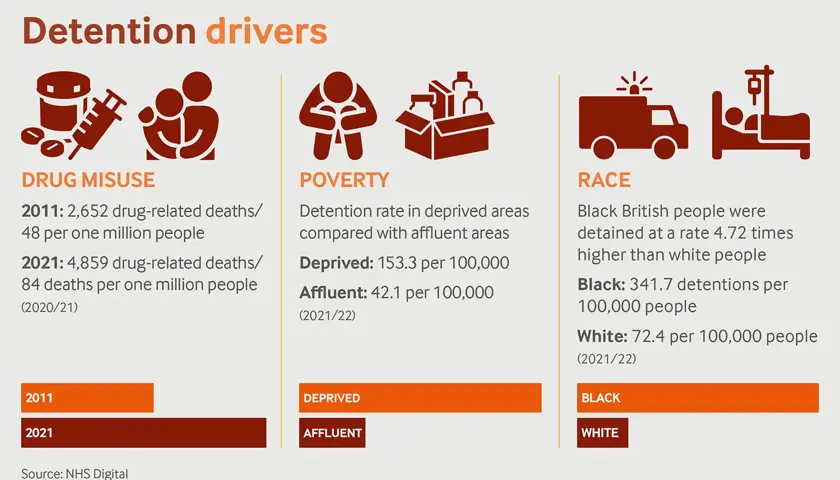
In 2021, the most recent year of ONS data, there were 4,859 deaths related to drug poisoning recorded in England and Wales, representing a rate of 84 deaths per million people. In 2011, the 2,652 drug-related deaths represented a rate of 48 per million people.
Dr Rhinds explains how community drug teams that existed in the 1980s would often treat ‘dual-diagnosis’ patients outside of psychiatric services. Now, the landscape means GPs and other non-specialised doctors are being asked to deal with addiction on top of their current jobs.
Deprivation driving detentions
Systematic cuts and a dismantling of community services and early intervention have played a big role in this escalation, with the environments young people grow up in having a huge impact on their chances of developing mental health conditions.
Rob Poole, professor of social psychiatry at Bangor University, who held NHS consultant posts in Liverpool and North Wales for 21 years, is the author of a book called Mental Health and Poverty.
He says there is ‘no question’ of a link between income inequality, adversity and major mental illness, particularly inner-city poverty.
‘It is about social factors,’ he explains. ‘We’ve known this for decades, but we’ve ignored it’.
His thesis is borne out in data, our analysis finds, with people in the highest areas of deprivation detained at a rate more than three times higher than people in the lowest areas of deprivation (153.3 per 100,000 compared to 42.1 per 100,000) in 2021/22. And in the three years since this data has been recorded, the largest increase in detentions has been seen in the most deprived areas.
Prof Poole says: ‘There’s an almost linear relationship between deprivation in childhood and the chances of developing schizophrenia as an adult. And that’s compounded by the fact that current adversity has a very major impact.’
This, he says, is exacerbated by ‘a destruction of social infrastructure’ through over a decade of austerity policies. Increased demand, he adds, is ‘not because of an increase in psychosis’ but because ‘people are doing a lot less well’ – in part because it is now ‘more difficult being poor’.
Dr Smith says ‘a significant proportion’ of patients, particularly in more acute services, ‘have horrendous, complex stuff that happened to them when they were younger’.
Dr Raleigh agrees austerity has played a role but says the factors at play also ‘pre-date’ the 2010 Conservative government and ‘raise some very worrying issues’ – namely higher rates of detention among ethnic minorities than white people.
While 72 per cent of the detentions where ethnicity was recorded in 2021/22 were white, Black or Black British people were detained at a rate 4.72 times higher (341.7 detentions per 100,000 people compared to 72.4 per 100,000).
Dr Raleigh argues societal factors such as a lack of social support and deprivation can also be contributory factors.
Dr Smith says: ‘People sometimes mistakenly think racism [only] comes in at the point the person gets sectioned.’ Instead, she suggests ‘the point at which the discrimination happens is much earlier’, in deprived communities.
Police role
Another ongoing debate is the role of the police in mental health act assessments and detentions. Police, under sections 135 and 136 of the MHA, can take people to a ‘place of safety’ so a mental health assessment can be carried out.
There has been a 52 per cent rise in civilian detentions following the use of a place of safety orders between 2016/17 and 2021/22, with 3,982 in the last full year of data, suggesting a growing reliance on police attending emergency calls.
Yet that could be set to change with the announcement of the Right Care Right Person (RCRP) scheme in July, which aims to reduce the number of mental health emergencies officers are called to while apparently ensuring they still respond when there is a real and immediate risk to life or serious harm.
Announcing plans for The Met, commissioner Mark Rowley said the force was ‘failing Londoners’ by sending police officers rather than mental health professionals to those in crisis as well as ‘taking large amounts of officer time away from preventing and solving crime’.
Ms Cheney was part of the expert reference group consulted on RCRP. She says ‘at face value, the goal is a reasonable one’ because police are ‘often called to and left with situations that can and should be managed by another agency’.
But she warns of some situations where police officers are ‘the only ones who can help’ and fears forces may use RCRP ‘as a way to say no’ to any mental health request.
Sir Robin says he ‘understands’ the moves and that society ‘can’t expect the police to take the place of psychiatric services’.
Many doctors and experts are, however, concerned about the risk and pressure on health professionals amid an existing workforce crisis, and among some there is a sense that the police may just be giving up on some of the most vulnerable in society.
Dismantling of services
Away from the involvement of the police, doctors are near-unanimously concerned about the breakdown of societal services and public health interventions which have previously stopped people from becoming so unwell.
Dr Bicknell says the breakdown in community care, and wider austerity witnessed over the last decade or so means ‘we are a society dominated by depression and anxiety.’
He says structures have broken down, GPs don’t have enough time to properly assess sick notes and benefit centres are ‘cut to the bone’.
‘Patients don’t get the appropriate medical and humanistic support and care they need to recover,’ he adds. ‘They are encouraged to remain entrenched in whatever situation they are in. It is all just so badly broken.’
Prof Singh highlights the closure of day hospitals offering therapeutic services where patients can be monitored closely without being detained or staying overnight, giving families ‘respite’.
‘All those softer elements have been removed along with the beds for when you are more seriously ill,’ he says. ‘We are not able to help patients early enough.’
Ms Cheney adds: ‘Austerity has decimated community mental health and many other social and community resources.’ She says mental health conditions ‘are a product of people's lifestyle, their experiences of poverty, oppression, educational situations’.
And while she would welcome a better-staffed mental health service with more beds, she thinks the root problems can only be addressed when decision makers look at recovery as ‘recognising where this comes from’ and fixing environments for when patients are better.
Philip Timms, a consultant psychiatrist at South London and Maudsley, specialises in the links between homelessness and mental illness, which he says is a ‘two-way’ issue, with psychosis both a potential driver of homelessness and homelessness exacerbating serious mental ill health.
Prof Timms says ‘the most destructive thing’ among the plethora of austerity brutality was the dismantling of Sure Start centres ‘because that's where you've got the greatest ability to make the greatest long-term impact’.
‘We know all sorts of health outcomes are related to social inequality, deprivation, abuse and neglect. If you can start to reduce that early on, you've got a chance of reducing the future load on not just mental health services, but physical health services as well,’ he says.
Less of everything
Dr Molodynski says: ‘There are high levels of patients with drug, alcohol, mental health, and gambling problems, who are often being endlessly passed around stretched services that say they should be treated elsewhere without much treatment actually happening for many, which must be immensely frustrating.
‘The division of services is a Catch 22 in that substance misuse services might say you need to see mental health services, and then your psychiatrist might say they can’t do much about your depression until you sort out your drinking.
‘Common sense has gone out of the window, and the end result is distressed people being at risk for much longer and probably costing the NHS more long-term.
‘Sadly, there's less of everything. People have less of a personal safety net in terms of finances and informal social networks. Core social services have been cut and there's less available in terms of what charities can do.
‘People are desperate and it’s spilling out through the system, be it presenting in more acute crises or turning up to A&E because there’s nowhere else to get help.’
People are desperate and it’s spilling out through the system, be it presenting in more acute crises or turning up to A&E because there’s nowhere else to get help
Dr Molodynski
The BMA is calling for a sharp increase in funding for mental health services and staff which accounts for the sharp increase in demand on top of increasing the £2.3bn promised per year from 2023/24 against inflation.
In addition, the association says there must be increased investment in primary care, public mental health, mental health research, and the mental health estate, acknowledging the importance of all the roles in mental health treatment.
Prof Burns brings it back to that crucial model of continuity of care, which he says is ‘vastly more important’ to mental health than physical health.
He wants clinicians to have more autonomy to create multidisciplinary teams that can get to know, and keep in touch with, patients. Those relationships between clinicians and patients are of the utmost importance, he says.
Neither Prof Burns’ expertise nor motivation are in much doubt. Improving the system is about preventing illness and saving lives. The potentially unnecessary suffering of every extra patient who becomes so unwell that they need an MHA assessment is a tragedy which also increases the burden on services and staff and, ultimately, the risk of mistakes.
Even in retirement he has never forgotten that 22-year-old art student and the three or four times he ‘got it wrong’.
Additional work by Claire Chivers and Olivia Clark