Resume the war on plastic waste
Plastic is a vital weapon in infection control and has never been more so than during COVID. However, the World Health Organization warns COVID-related plastic waste is itself a threat to human health. Have we reached a tipping point?
Suspending the war on plastic waste was seen as a necessary evil to tackle a global health emergency. PPE (personal protective equipment), testing kits and vaccine syringes were essentials in the fight against COVID: how to dispose of all that plastic was a question neatly sidestepped.
Yet, two years on, the statistics about COVID-related plastic waste are shocking. Globally, an estimated 129 billion face masks and 65 billion gloves have been used each month during the pandemic – 75 per cent of which will end up in landfill or the ocean, says the WHO. The NHS alone used an estimated one billion surgical masks in the 12 months from February 2020.
In March, Dutch researchers detected microplastics in human blood and tissue for the first time. Plastics have been a defence in this pandemic – and some remain essential – but could we do things differently? Many doctors insist we can and must do much more, starting now, to end our reliance on single-use plastics – and switch to more sustainable practices and systems.
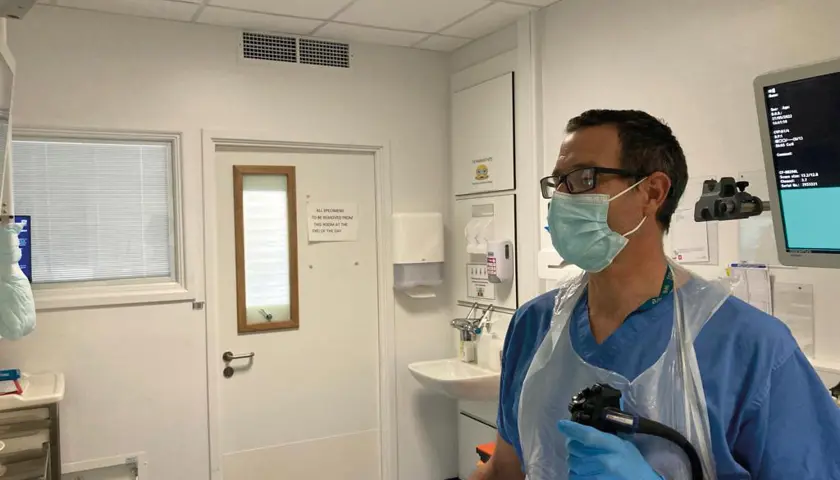
It will take creativity, innovation and big-picture boldness, but alternative solutions are possible, they believe. Bill Stableforth is a consultant gastroenterologist in Cornwall and climate activist.
‘If the pandemic has shown us anything, it’s that given a bit of space to innovate, we can make changes fast,’ he says. ‘NHS staff and others can turn a service on its head, this afternoon even, with a little help.’
Set a target
Some of these steps are relatively straightforward – yet many large NHS organisations are still not taking them.
The BMA has called on trusts and health boards to have ‘policy and an ambitious target’ to reduce single-use plastic waste and to explore re-use options for medical equipment, such as sterilisation.
It’s also called on the Government to help the NHS achieve these and other sustainability goals. Almost a quarter of the NHS’s waste in England and Wales is plastic, says NHS Supply Chain.
Yet, BMA research in 2020 found that the nearly six in 10 trusts in England reported having no policy to deal with single-use plastic.
Even recycling of non-infectious waste is poor. Studies vary but it’s estimated that as much as half of the NHS clinical waste stream – mostly bound for incineration – could be treated as domestic waste.
Marina Politis, a medical student on an intercalated degree in Scotland, voiced her frustrations about the lack of waste segregation in healthcare settings at the BMA annual representative meeting last year.
‘So often everything is shoved in the same bin: there’s no sorting,’ she says. ‘The least we can do is recycle: that’s a very small step.’ Abi Carey, a specialty trainee 5 registrar in geriatric and general internal medicine on Merseyside, has regularly taken recyclables home to add to her household bin and even provided an informal recycling bin at work.
Where recycling facilities do exist, she says, they tend to be poorly labelled or misused. But Dr Carey, who is passionate about low-waste living at home and had a low-waste wedding last month, makes an important point.
‘It’s currently very difficult to uphold or promote more sustainable practices in the NHS, because many staff are burnt out. It feels like there is no brain space for people to take on new challenges and changes.’
Re-use revolution
Some trusts are ‘making it easy for people to care’, as Ms Politis puts it. Royal Cornwall Hospitals NHS Trust, where Dr Stableforth works, is a pioneer in this space. During the pandemic, the trust invested in a Sterimelt machine to divert plastics away from incineration.
It uses heat to turn face masks and other plastics such as theatre tray wrap into polypropylene blocks. The trust has worked with a local firm to turn these blocks into litter-pickers, donated to every local school and college. Win-win.
The statistics about COVID-related plastic waste are shocking
Dr Stableforth
RCH is also part of a national trial, across several NHS sites, of the world’s first net-zero clinical laundry service for gowns, aprons, coveralls and surgical masks. An early study found that it had the potential to save the NHS an estimated £9m a year.
‘We shouldn’t talk about “waste” and “throwing things away” because there is no such thing as “away”: these are valuable resources,’ says Dr Stableforth. ‘People want to do the right thing but hospitals and the NHS have to facilitate that.’
Other initiatives are coming on stream. Recycling schemes for clean PVC medical devices such as anaesthetic masks, oxygen masks and tubing were being trialled in several trusts before the pandemic.
Some manufacturers are starting to use biodegradable materials such as compressed hemp for medical textiles and masks. In Australia, trials have even seen face masks combined with processed building rubble to be used in road construction.
Gloves are off
To reach the NHS’s sustainability targets, the war on single-use plastics needs to resume, with urgency. As recycling and reusing need infrastructure in place for repurposing or sterilising, the ‘reduce’ mantra is gaining traction. Part of this offensive will have to include tackling ‘unnecessary and overuse of PPE’, says the WHO.
The Royal College of Nursing’s recent Glove Awareness Week, which the BMA supports, encourages healthcare professionals to be more discerning in their use of plastic gloves.
A pre-pandemic campaign at Great Ormond Street Hospital encouraged staff to stop using non-surgical gloves where handwashing would suffice. This saved the hospital 21 tonnes of plastic and £90,000 in just 10 months.
With good hand hygiene, glove use is not necessary for vaccination, the WHO says, yet ‘this appears to be common practice’.
Ms Politis, who campaigned in Glasgow during UN climate talks COP26 last year, was dismayed to see 300 medical student colleagues donning and disposing of plastic gloves at each one of eight assessment stations during recent exams. More joined-up thinking could help address other types of waste too, she says.
‘Intubation equipment on the resus trolley was being thrown away a month before its use-by date so I asked if it could be taken to A&E where it would be used immediately, but was told: “Policy means we can’t”. Perhaps policies need to change.’
Cannulations were routine in emergency departments at St Mary’s and Charing Cross Hospitals until it was discovered that more than 40 per cent of cannulas inserted upon attendance went unused. Education and awareness campaigns reduced cannulation by 25 per cent in a year, saving £95,000.
As part of a ‘Green Surgery Challenge’ run by the Centre for Sustainable Healthcare, a pilot by Leeds Teaching Hospital NHS Trust focusing on laparoscopic appendicectomy found that simply inviting patients to visit the toilet before the anaesthetic room eliminated the need for urinary catheterisation.
Momentum for change
The future of plastics is uncertain, with the global fuel crisis threatening oil-based production.
New technologies such as plastic-eating ‘super-enzymes’ are causing excitement.
Dr Carey insists that plastics cannot be seen in isolation from the wider climate crisis – and not just because solid waste treatment and disposal accounts for 5 per cent of global emissions.
Human and planetary health are inextricable. As she puts it, ‘eventually, nothing will matter except the climate’. Dr Stableforth agrees: the plastic crisis cannot be allowed to detract from more pressing ‘big-ticket items’ such as reducing emissions. ‘We need big change in big systems,’ he says.
People want to do the right thing but hospitals and the NHS have to facilitate that
Dr Stableforth
His trust declared a climate emergency two years ago and works with other trusts in moves towards sustainability. Building momentum for change is vital, says Dr Stableforth, with doctors using their position of authority and influence and the NHS leading by example.
He’s keen to see healthcare settings becoming ‘anchor institutions’, large employers and procurers that model and encourage sustainable practice.
‘If a hospital divests from fossil fuels, procures in an ethical and environmentally friendly way, focuses on active transport, rethinks its food, all that has a ripple effect throughout the local community. Hospitals need to use their leverage and it’s not happening fast enough.’
Patients' plans
Ms Politis would like to see sustainability embedded into more medical schools’ curriculum – and into clinicians’ conversations with patients.
‘We should be talking to patients about their environmental practices as part of their health profile,’ she says.
‘But how can we do that if they’re being treated in a setting which doesn’t care about waste and the environment?’ Dr Stableforth remains determinedly optimistic.
‘I think people worry about climate action, because they think they’re going to have to live in a mud hut and eat raw turnip. But by phasing out fossil fuels, having active transport for all, the ability to walk and cycle to places with clean air, car-free cities… the social, psychological and physical benefits are just enormous. The solutions are beautiful.’
Illustration by Simon Grant