Mental health: no locks, no stigma
A new initiative to create safe, supportive spaces for those with mental health conditions could help spare some the trauma of being admitted and detained
‘I’ll never forget the first time our daughter was sectioned,’ says Ros Savege, a mother and carer of a woman with complex and co-morbid mental health conditions including schizophrenia and enduring psychosis.
‘The driveway was full of cars: lawyers, approved mental health professionals, psychiatrists, police and others. All of a sudden, all these people arrived. It’s the only way the system worked.’
As a member of York Mental Health Partnership, Mrs Savege has been a leading voice on a project to transform mental health services in the city. One of its aims is to reduce the likelihood of experiences such as her family faced one of the three times her daughter was detained under the Mental Health Act.
York’s Connecting our City project was recently awarded £2.4m from NHS England to develop a 24/7 community adult mental health hub.
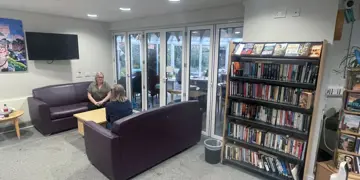
Its vision is of holistic, wrap-around care at any time of day or night, providing a safe space for those with mental health conditions with no locked doors, no discharge and no stigma.
People get support with everything around them in their life as well as the interventions
Dr Wright
There will be no need for a referral to the hub, which will operate alongside existing psychiatric hospitals and crisis services, with the aim of reducing the likelihood of people reaching a stage where they need to be formally admitted or detained. It hopes to provide support for those in distress, looking at the societal context of their needs.
Funding for the hub has been awarded after a successful pilot scheme, which will continue to operate. A third site in the city is also planned.
York’s transformation has been heavily influenced by the Department of Mental Health in Trieste, Italy, which pioneered a ‘whole person, whole life, whole systems’ approach to mental healthcare in the 1970s – in response to concerns about the use of asylums.
The Trieste model is backed by the World Health Organization and described as an ‘open door, no-restraint system of care for recovery and citizenship’.
Rather than focusing on clinical symptom reduction, it prioritises dealing with the social context of patients’ conditions, fostering a sense of belonging, safety and inclusion under the mantra ‘Liberty is therapeutic’.
Holistic offer
Over the decades in Trieste, there have been recorded drops in the number of mental health inpatients and emergency presentations, the number of involuntary treatments, incidents involving people with mental health conditions and law enforcement, as well as the suicide rate. Meanwhile, more people with mental health issues have been supported into employment.
Clinicians in York hope to replicate this as they further roll out the approach they’ve been working on since the closure of local psychiatric hospital Bootham Park in 2015, which originally opened as the ‘county lunatic asylum’ in the 18th century.
Consultant psychiatrist Stephen Wright, an independent co-chair of the York Mental Health Partnership, casts his mind back to before transformation work began: ‘There was something of a crisis of services in York, where the fragmentation of the system and insane paradoxes played out.’
Explaining the principles of the new model, he says: ‘Traditional mental health services have an access team, which offers some governed interventions, which people have to wait for. But by coming here they not only don’t have to wait, but they also get a more holistic offer – they get support with everything around them in their life as well as the interventions.’
Fellow co-chair Lynne Gabriel, a professor of counselling and mental health, explains how the project required ‘really dedicated people’ to ‘push at the doors of an antiquated system’ in the early stages.
‘There is no revolving door,’ she says of the community approach. ‘People come through one portal, access a compassionate human being and receive support with whatever they are presenting with. It was really important to stop that process of saying, “I can’t help you here, go over there”, that constant shifting of someone round a bigger system.’
The hubs will be run by a multidisciplinary team of clinicians, social workers, social prescribers and peer support workers from the NHS and voluntary sector.
‘There’s no pitting a medical model against a social model, we all work together,’ says Prof Gabriel. ‘But we do need that medical input.’
Early intervention specialist Dr Wright adds: ‘There’s always a danger of over-medicalising things. For GPs, in the traditional model, it would often be a referral or a prescription rather than an opportunity to have a closer look at someone’s needs or whole life.
‘Some things my team can do better than me, which is important for a doctor to acknowledge. But there is of course that need for prescribing and medical cover at all times.’
High engagement
Measuring outcomes could take ‘generations’, he says, noting the importance of having created a clear and co-produced set of principles. But results of a prototype study show early successes.
Of 33 service users, only one did not engage. Some 24 reported progress with the reasons they sought support. Service users reduced their drug and alcohol use, were given support with housing and benefits, had their medication reviewed and had neurodevelopment screenings.
Dr Wright says more than 50 per cent saw ‘significant clinical improvements, without any medical or clinical interventions’, meaning ‘non-clinical interventions improved clinical outcomes’, something they hope to ‘explore further’. Some have moved into paid peer support worker jobs at the hub.
It was really important to stop that process of saying, 'I can’t help you here, go over there'
Dr Gabriel
For Mrs Savege, the pilot (which opened in 2023) has been ‘a very different experience’ for her and her daughter, which she is sure the 24/7 hub will build upon.
‘We were living in absolute hell, despite a lot of support,’ she says of previous care. ‘Our daughter would be going from A to B to C. She would shut down because it used to be “who is it today?”, “where are we today?”, which added so many layers of disempowerment.
‘She doesn’t open letters, use a phone or use a computer, and that’s not unique. Elderly parents can be the only people getting their adult children to an appointment, or clozapine clinic.
‘Services might be getting these people stable, but they’re under the radar. They’re medicated, they’re not overtly psychotic, so job done. But it does not provide any quality of life.’
Mrs Savege describes the ‘barriers’ and ‘blockers’ in traditional mental health systems, where patients are ‘siloed’ and ‘labelled’.
‘It’s shocking, but you need a label to open doors,’ she says. ‘Who would like a label of schizophrenia?’
In contrast, the community hub offers ‘a system which talks to each other and is co-ordinated’ with ‘one door to walk in with somebody there to help you’.
‘There are no locked doors, no lanyards, we never signed in. When you walk in you don’t [immediately] know if you’re talking to patients, carers, support workers, psychologists. That openness builds relationships for somebody like our daughter, who doesn’t feel like she belongs to any community.
If you can’t use coercive or restrictive techniques, you just have to do it differently
Dr Wright
‘Everything is about relationships and trust, and so much more so when you’re very unwell because the challenges of new people and new faces are so much greater.
‘It’s [also] about having confidence. If you know something is there, very often you don’t access it. You don’t need to escalate when a service is there, rather than feeling like there’s nowhere to go.
‘When you have complex issues, you need a broad support network. I don’t know what my daughter experiences, I’m not sure even she can describe it, but it’s a complete sense of otherness. You lose your friends, your contacts, you are stripped down to nothing, really, by very serious mental illness. Society has to find a way of filling enough of that gap.’
Risk assessment
Dr Wright agrees that difficulties can be ‘compounded’ when there is less support for those with mental health conditions, particularly out of core working hours.
He says the biggest challenge for clinicians in switching to a Trieste-style model is reassessing their approach to risk.
During the group’s second fact-finding visit to Trieste, Dr Wright recalls then-director Roberto Mezzina explaining ‘if the door is locked, the doctor is free; if the door is open the doctor is responsible’.
That take is in line with Italian Law 180, also called the ‘Basaglia Law’ after psychiatrist Franco Basaglia, who led reforms in Trieste. The law stipulates that admission to hospital be allowed ‘only if it can be shown that community-based treatment options are not feasible or have failed’.
‘We went with a really critical eye, thinking “how can we make this work?”,’ says Dr Wright, noting the differences between Law 180 and the UK’s mental health act. ‘If you can’t use coercive or restrictive techniques, you just have to do it differently,’ he says. ‘We asked, “what do you do when someone is seriously intent on harming themselves?” Ultimately, you find a way, and the more collaborative it is the better.’
Dr Wright has since followed this principle in clinical practice when dealing with what ‘are often insoluble problems’. He says: ‘If everyone can talk it through and agree a way forward, then if something goes wrong it’s not because everybody hasn’t had an opportunity to contribute.
‘Things go wrong anyway. But there’s still a culture where organisations don’t want to take on risk. If they can keep the risk at arm’s length, then they don’t get in trouble. Ultimately, that risk doesn’t go away, it just remains in the community – and sometimes it plays out even worse.
‘So the responsibility [should be] for all organisations to actually recognise it, roll their sleeves up and collaborate.’
The York hubs will offer outreach as well as an open door. This could be for service users who haven’t shown recently, or potentially vulnerable people for whom there are concerns.
‘If you’re not getting the help you need, you tend to escalate,’ says Dr Wright. ‘Then things get worse because the way the system operates [traditionally] is that you need to reach a certain threshold before you get help. That shouldn’t be happening.’
Prof Gabriel explains how it is often frustration at the system, and a sense of rejection, that causes people to resist treatment and lash out.
She explains how the pilot hub worked with a service user who had ‘a long history of disturbances with the police’, had been homeless and ‘written off by social services’.
‘They misbehaved a little bit, but the team reached in to connect with that individual and very gradually relationships developed. They showed compassion, care and acceptance.
‘There are some limits, of course – you can’t bash staff in the teeth – but within that there is huge liberty to explore being in relationships with human beings who are accepting. An individual like that can find their feet in these loving relationships.
‘There’s something profoundly precious about coming across a human who looks at you, might touch your shoulder or be willing to have a cuppa with you. That, for some people, is so different from what they’re used to.’
Prof Gabriel also notes ‘clear indicators’ of potential NHS cost savings by taking preventive action, though insists that would be a ‘byproduct’. ‘We’re not doing this for savings, we’re doing this for people,’ she says.
Mrs Savege adds that some people who are currently ‘invisible’ to traditional mental health services may also be more likely to engage with the community approach. ‘Nobody has been interested in the root causes before,’ she says.
York has a proud history of innovative mental health services. In 1790, prominent Quaker William Tuke opened The Retreat, a humane alternative to the asylums of the day after concerns were raised about the treatment of a patient who died in care.
The Retreat still operates on the same site today, as an independent non-profit commissioned by the NHS to provide autism and ADHD diagnostic assessments.
Alyson Scott, chief executive of York Mind, said the relationship between statutory bodies and the voluntary sector in the project ‘actually feels like a partnership’, with its staff feeling empowered to help service users which can also free up psychiatrists’ time.
‘We can transform a system to make it better for people using it, without there being huge implications on cost. This is a genuine shift towards mental health services being more responsive to the needs people have, and we could be sat here in 20 years talking about how we were very much at the forefront of that.’
Claire Douglas, leader of York City Council, said she was taken by the Trieste model’s principle that ‘the community looks after the community’.
‘I’m tremendously supportive of mental health services that deliver for our residents when they need it in a way that makes sense for them and feels accessible for them. Our data and the response of the people who have used the services so far have shown that it does really work.’
‘York is a social justice-driven city, that’s our history. People here do look out for each other, they do care about their neighbours. I don’t think our citizens would expect us to deliver mental health services any other way.’
The vision is to have a mental health system we’re proud of
Dr Wright
A recent HSSIB (Health Services Safety Investigations Body) report found that many mental health services are being run in ‘dilapidated’ facilities. It recommends ‘making therapeutic care a priority’. The new Labour Government has set out its intention to transform the NHS into a more preventative system.
York’s Mental Health Partnership hopes its mental health services can become a model for others to emulate, and says it aligns with recommendations from the Hewitt review and Darzi report.
Prof Gabriel says: ‘If we have enough evidence to show this is making a difference, then if more money becomes available, this could be the beginning of a movement. There have been seeds of this for a long time. People are beginning to notice that there’s a different way of doing it.’ Dr Wright adds: ‘They’ve been talking about it for decades, the only thing that hasn’t happened is actually implementing it. We have to demonstrate you can do that, and fund it adequately.
‘The vision is to have a mental health system we’re proud of. That’s what we saw in Trieste. There’s a lot of passion. They were showing it off. We want to do that too.’
(Photos by Ben Ireland)