Life in colour
Life in colour
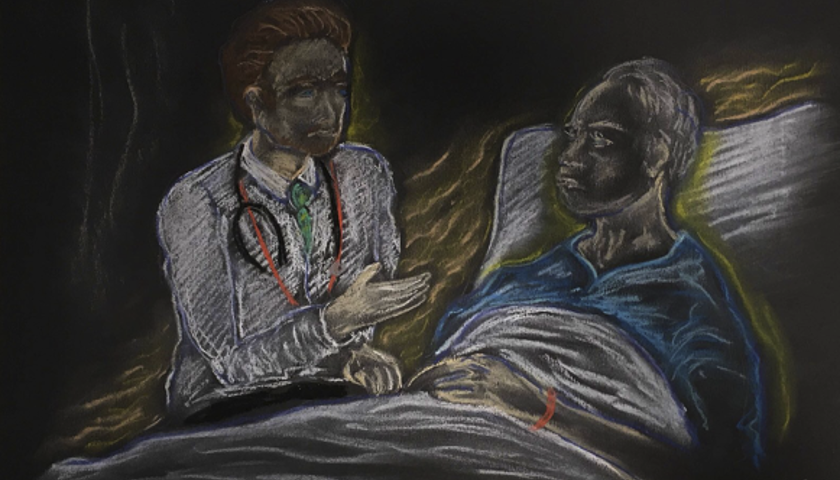
The use of art therapy to aid recovery or treat trauma has helped patients and doctors alike to the extent that many professionals now advocate offering it more widely on the NHS
‘I found I could say things with colour and shapes I couldn’t say any other way – things I had no words for.’
Ground-breaking female artist and pioneering figure of the American Modernist movement Georgia O'Keeffe’s assessment of her relationship with her art perfectly illustrates the power of creativity with regards to self-expression.
In whatever form it might take, art plays an important role in the lives of most people, who value it for the enriching, enlightening and sometimes provocative effect it can have, or for the simple fact it has the capacity to bring joy.
While appreciating and creating art can undoubtedly play a role in improving our wellbeing, the role it can play in health and medicine is often complex and poorly understood.
The name ‘art therapy’ is familiar to clinicians and patients alike having been used for more than half a century in healthcare. However, it is often applied in loose and ill-defined terms.
I attribute a lot of my recovery to the creative therapies that I had access to
Dr Dosani
While engaging in creative activities, such as joining an art class or choir can form part of social prescribing, art therapy refers to a form of psychotherapy which uses art creation as a form of treatment in its own right or in addition to other elements such as CBT and talking therapies.
The British Association of Art Therapists describes art therapy as ‘a form of psychotherapy that uses visual and tactile media as a means of self-expression and communication’.
Delivered by accredited art psychotherapists, art therapy has been used in conjunction with a wide range of illnesses and medical conditions and can centre around a variety of mediums from visual art to dance, drama and music.
As a form of treatment, however, art therapy is not without its detractors with some criticising the historic lack of an evidence base as to the efficacy of using art therapeutically when compared with more traditional forms of treatment.
Consultant child and adolescent psychiatrist Sabina Dosani has a professional and personal appreciation of the benefits art therapy can yield.
As a medical student, Dr Dosani was for a time hospitalised with depression at Guy's Hospital in London. During her stay she received group-based art therapy alongside talking therapies as part of her treatment.
Despite being a medical student, she says it was the first time she had ever encountered art being used therapeutically.
‘I just thought that was a normal part of treatment, I didn't realise how unusual that was,’ she explains.
‘It really helped me put certain things into a form of communication that I hadn't been able to articulate, and it helped me to form a sense of identity.
‘When I looked at the paintings, when I was discharged, I realised how my life had increasingly become more colourful, and I really attribute a lot of my recovery to the creative therapies that I had access to.’
After gaining her medical qualification, Dr Dosani again found herself finding success with art therapy after being diagnosed with postnatal depression.
Dr Dosani’s experiences led her to undertake a master’s degree in medical humanities and to begin considering what role arts-based interventions could play with some of her own patients.
A consultant child and adolescent psychiatrist, Dr Dosani is also involved in medicolegal work and serves as an expert witness to the family courts and asylum cases involving children and young people.
‘When I’m assessing children, I don’t think of that as art therapy, but as using arts basically as tools to help with engaging with assessment,’ she says.
‘I see a lot of young people who’ve crossed in small boats or had trauma from coming from conflict. We often don’t have language in common, but there’ll be an interpreter, [and I] invite them to draw whatever is in their minds.
‘They very typically will draw detailed scenes of the kinds of difficulties and adversities they've experienced, they might draw pictures of abuse, graphic representations of war or pictures of the camps they’ve been in.
‘That feels like a much richer description than asking open-ended questions as a stranger through an interpreter,’ explains Dr Dosani,
‘It breaks down one of the communication barriers, and those pictures do become part of your clinical record, they help to evidence things like post-traumatic stress disorder when these cases go to immigration and asylum courts.
‘It’s a really useful way of getting clinical information, but for some children those assessments are [also] therapeutic, as it’s the first time they’ve been able to put down something on paper and have an adult witness it and care.’
There’s something about art making that gets to the heart of things
Dr Dosani
While art therapy has existed in one form or another in healthcare since at least the last century, as a form of treatment it has sometimes faced criticism for the paucity of evidence underpinning it.
While Dr Dosani accepts arts-based interventions in healthcare cannot be viewed as a panacea, she believes the evidence base for the efficacy of art therapy is growing, with numerous studies and systematic reviews having been undertaken.
Clinical research fellow Megan Tjasink, is hoping her work examining the use of art therapy as a means of addressing burnout among healthcare professionals in secondary-care settings, will further bolster the case for art therapy.
Having served as the lead art psychotherapist at Barts Health NHS Trust’s cancer and palliative psychological services departments, Dr Tjasink has been leading the CHArt group art therapy intervention as part of a randomise control study at Queen Mary University of London.
The study, which grew out of an earlier project delivering art therapy to staff in Barts’ oncology teams almost a decade ago, involved getting different healthcare professionals together, including doctors, to participate in making art and encouraging discussion.
Deeper level
Dr Tjasink, who aims to publish the findings of her research later this year, says she hopes art therapy can become an established and more accessible form of treatment in the health service.
‘In the last couple of decades there has been huge growth of art therapy within educational settings, especially in child and adolescent mental health services,’ explains Dr Tjasink.
‘I wanted to create an intervention [for healthcare professionals] that fit around their work schedule and so developed a six-session art-therapy intervention based on themes pertinent to burnout and using the Maslach burnout inventory.
‘There’s something about art making and creative expression, that gets to the heart of things. You're connecting with feelings on a deeper level than you would if you were just using sort of your intellect or cognition.
‘[The participants] enjoyed having a sort of non-judgmental space where they could share their difficulties and support each other, but there’s also something about the creative process, and art making and being able to express yourself in a different way.’
Anaesthetic registrar Denise Gomez is one of about 50 doctors who participated in Dr Tjasink’s study.
She says she was drawn to the project for a number of reasons including having enjoyed art and creativity in her personal life, wanting to contribute to research and the ease with which she could access the programme.
Even though she went in with an open mind, Dr Gomez says she was genuinely surprised by the effect creating art had for her and those around her and would now love to see art therapy offered more widely across the NHS.
‘I think whether we call it stress, burnout, depression, any other clinical names, I just feel like, nearly everyone in the NHS is struggling in some way or another and it’s not something that’s going to go away anytime soon,’ says Dr Gomez.
‘I’ve had other forms of therapies over my life like talking therapy, breath work and yoga. Each has its own value in its own worth, and every modality is different, but art therapy, and doing it in a group, was really valuable.
‘Even just in the first session [it] got to a level of openness and [confronting] difficult emotions I just don’t think would have otherwise happened in a room of basically strangers. There's something about that, using the activity of creating art that just lets people speak.’
Dr Gomez says that, unlike existing approaches to addressing burnout and an emphasis on health service staff developing resilience, participating in art therapy as part of a group felt individually liberating while also fostering a sense of solidarity with colleagues.
‘Wellbeing and resilience are words that get kind of used as a bit of stick to beat us,’ Dr Gomez says.
‘It’s become this very top-down concept, where we’re told “you have to do this and that and the other” to maintain your own wellbeing.
‘Art therapy is the reverse. It doesn’t feel top down because you’re being allowed to express yourself as an individual. You’re given this opportunity to create and to feel a sense of self which often gets lost in a very big institution like the health service.
‘Staff often feel like numbers, and I think when this happens it’s easy for them to treat patients like numbers. Having the opportunity to do something truly for your own wellbeing really distinguishes art therapy from any of the other initiatives I’ve seen in hospitals.’
Listen to a podcast which builds on this feature