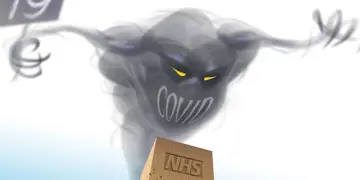
Austerity - Covid’s little helper
Severe public health cuts left the UK more vulnerable to COVID – while the huge bill from tackling the pandemic could make austerity even worse. Peter Blackburn reports on doctors’ determination to break a vicious circle of decline.
Heather Grimbaldeston was used to having to balance the books – all too familiar with making ‘the public purse stretch’. But, as director of public health for Cheshire East in 2016, it was simply no longer possible.
Years of brutal cuts to public health services, following NHS reform legislation passed in 2012 which moved public health from the NHS to local authorities whose budgets were hit the hardest, had taken their toll.
‘I’ve always worked in areas which are under-resourced – I’ve done it and I’ve done it with the support of great colleagues and under difficult circumstances,’ Dr Grimbaldeston says.
The years were tough. Mental health support services, smoking cessation support and sexual health services – among many others – suffered ‘extreme cuts’. Staff numbers dwindled and health protection, let alone health improvement, became notions of fantasy rather than reality. And eventually, it told. ‘I couldn’t make it work any longer,’ she admits.
It has been heart-breaking to see the neglect of public health.
Dr Grimbaldeston
Former director of public health for Stockport Stephen Watkins can identify with the experiences of Dr Grimbaldeston. He says: ‘It has been heart-breaking to see the neglect of public health. I only retired about a year ago and for the last couple of years before that we had been trying to find ways to minimise damage. You couldn’t develop and extend services, you were in the business of trying to minimise damage.’
This bleak landscape was not isolated to these two areas of the North West. Nationally, local authority budgets were cut by nearly a third from 2010 to 2018, according to the National Audit Office and the public health grant fell by £700m in real terms between 2014/15 and 2019/20, as revealed by a Health Foundation report.
Across society a decade was defined by the destruction of a safety net built over many years. From the closure of Sure Start centres and libraries to the crumbling estates and rocketing vacancy lists of NHS organisations – few public services were left unscathed.
The results of these political decisions have been damning. Life expectancy across England has stalled, the inequalities in life expectancy between the most and least deprived areas of the country have increased and the amount of time people spend in poor health has increased. At every step along the way doctors have felt the strain – whether in rocketing demand from patients or increasingly impossible working environments.
‘Health is telling us something fundamental about the nature of society,’ University College London professor of epidemiology and public health Michael Marmot tells The Doctor. ‘If health stops improving it means society stops improving.’
Austerity's shadow
As Sir Michael’s landmark report in February, 10 years on from the Marmot review of 2010, said: ‘From rising child poverty and the closure of children’s centres, to declines in education funding, an increase in precarious work and zero hours contracts, to a housing affordability crisis and a rise in homelessness, to people with insufficient money to lead a healthy life and resorting to food banks in large numbers, to ignored communities with poor conditions and little reason for hope… Austerity will cast a long shadow over the lives of the children born and growing up under its effects.’
In his final report on the impact of austerity in the UK, United Nations rapporteur on extreme poverty Philip Alston, was damning of politicians, accusing them of the ‘systematic immiseration of a significant part of the British population’ and said austerity had ‘deliberately gutted’ local authorities.
It is in these circumstances – in this seemingly broken Britain – that the response to the greatest public health threat in living memory was to be framed.
‘We were in a very bad state – and then came the pandemic,’ Sir Michael says.
He adds: ‘In 2009/10 public expenditure was 42 per cent of GDP and by 2019 that had become 35 per cent. That is significant. And that reduction in public spending was done in a very regressive way, and this gets us closer to our lack of preparedness for the pandemic.’
Low capacity
So, what did this effect of austerity on the state and society mean for the pandemic response? Firstly, it seems clear that the capacity of certain levers of state to respond quickly as cases of COVID-19 rocketed were deeply hampered: public health specialists deeply cut in number and resource were unable to track cases once they moved into the hundreds, the NHS relied on temporary hospitals in conference centres and cancelled swathes of non-COVID procedures, PPE stocks were out of date and unsuitable for the job in hand and testing capacity was very limited.
London School of Hygiene and Tropical Medicine professor of European public health Martin McKee says: ‘Austerity had a number of elements – it was part of a package which included diminished government spending on social welfare and other related sectors and coupled with that was a hollowing out of the civil service, the instruments of state and a sustained under-investment in the NHS and public health.’
One of the most devastating parts of the relationship between austerity and this pandemic played out, during the very height of the crisis, in the country’s hospitals.
As the Institute for Public Policy Research recently found, the decade of austerity left the NHS ‘extremely fragile’ before the onset of the pandemic – with more than four in five English hospitals operating with ‘dangerously low’ spare capacity.
The ‘dangerously low’ capacity – the product of a decade of underinvestment in the face of increasing demand from increasingly complex patients – combined with poor staffing levels and a lack of crucial equipment like ventilators, provided a deeply concerning backdrop for a pandemic response. The result was a rushed response, in parts seemingly cobbled together, to avoid catastrophic death tallies.
And, ultimately, that meant doctors working in unfamiliar roles desperately trying to cope with rocketing numbers of COVID-19 patients in potentially unsafe environments, £1.5bn emergency funding for field-style Nightingale hospitals and wanton encouragement of hasty discharge from hospitals into care homes and the community to free up beds – encouraging a rapid spread of the virus. It was one disaster after the next.
And the knock-on effect was huge. In total around 2.5 million patients missed out on investigations, treatments and procedures as the National Health Service effectively became the National COVID Service. Beyond the cancelled operations and shelved treatments there was an added hidden impact, as revealed by a BMA study earlier this year.
It found that there had been up to 1.5 million fewer general and acute admissions, up to 2.6 million fewer first general and acute outpatient attendances, around 280,000 fewer urgent cancer referrals, up to 25,900 fewer patients starting first cancer treatments following a decision to treat and up to 15,000 fewer patients starting first cancer treatments following an urgent GP referral.
For doctors, it was a remarkably difficult time. In August a BMA tracker survey revealed that 35 per cent of doctors were suffering from stress, anxiety, depression or burnout worsened during the pandemic.
The reduction in public spending was done in a very regressive way.
Professor Marmot
It is probably unfair to attribute all of these problems to austerity politics – clearly responding to the spread of a disease with such great risk of transmission and fatality would always involve disruption, and indeed great change to the structure of services and facilities. However, there can surely be no question that the austerity politics of the 2010s left the NHS and the wider health and care system deeply hamstrung and simply hoping to avert total disaster.
Nowhere has the impact of austerity on the pandemic response been more obvious than in public health. The system – described by Dr Watkins and Dr Grimbaldeston as being a near-impossible environment – had been so decimated it did not have the resource to lead and run a pandemic response.
One public health consultant, who wished to remain anonymous for fear of repercussions if he spoke out, explains the struggles of public health to The Doctor.
He says: ‘The earliest thing was that by mid-March PHE (Public Health England) had been overwhelmed – all of its contact tracing capacity was entirely flat out trying to keep pace and that’s the point at which contact tracing stops and it was just about the time the World Health Organization was saying we need to test, test, test. The capacity of PHE had been run down over many years by austerity, we had cuts year-on-year on year, to the extent that the numbers of communicable disease consultants had fallen by about a third on where they were in the old days of the Health Protection Agency. We had lost a lot of expert public health specialist capacity over the decade of austerity and that certainly didn’t help.’
And when the Government decided significant public spending would be required to tackle the COVID-19 threat it placed its trust – and huge sums of taxpayer cash – in the hands of private firms such as Serco and Capita rather than investing in the structures of state decimated by a decade of starvation.
BMA public health medicine committee deputy chair Richard Jarvis says this leads to fragmentation and inefficiency.
Risk factors
While the implications of austerity politics hampered the UK response to the pandemic it has also influenced the very spread and impact of the disease.
This may be a novel disease but there already seem to be a group of major risk factors which make the coronavirus deadlier. Those factors include old age, pre-existing health conditions, ethnicity and low socioeconomic status. For example, it is now thought that COVID-19 can be about twice as deadly for the poorer among society.
We already know that austerity politics – changes to tax and welfare payments and the removal of the social safety net – hit the poorest in society the hardest. We also already know that health outcomes are the worst in our most deprived communities, and that those inequalities are getting worse. And now, the evidence suggests COVID-19 is doubling down on all of these tragedies – it is at its most deadly in the most impoverished communities and among those who already suffer the greatest health inequalities.
Those same health inequalities deeply exacerbated by the political decisions of the 2010s.
Dr Watkins says: ‘There are a whole host of problems that have come to light as a result of this. And the truth is that, although they have been highlighted and exaggerated by the pandemic, those inequalities exist in our society anyway, they have merely been exaggerated and brought to prominence by the pandemic. It also serves as a warning for where this country goes next if we look at the current state of health inequalities with much of that caused by policy over recent years.’
And Dr Grimbaldeston adds: ‘I think the pandemic has taught us that COVID has universally picked on and affected the countries with the greatest and most profound inequalities. There are some bugs that target various characteristics but I think if you had a tag that this bug held it would be that it targets the most disadvantaged, the least able, the least equal. The other thing it has highlighted is that in this country inequalities are everywhere and ingrained.’
And the relationship between austerity and this pandemic may continue into the future. Austerity set the conditions for the Government’s response and has clearly influenced the impact of the disease. With cases picking up and fears of a significant second wave growing, many will worry about the health and care system’s ability to cope without a major departure from the underinvestment of the past. It is a fear held by doctors, too. In the BMA’s August tracker survey half of doctors said they were not very, or not at all, confident in being able to manage a second wave of COVID-19.
If health stops improving it means society stops improving.
Professor Marmot
Perhaps most worryingly of all, given the UK economy has been the hardest hit among the world’s major economies – the economy contracted by 20.4 per cent from April to June and spending on the COVID response has taken the country’s debt to £2tn for the first time in history – there are fears that austerity will once again be the solution of a British government in times of financial crisis.
‘It’s absolutely essential as we come out of this that we think in a new way,’ Sir Michael says. ‘I wouldn’t start [designing the path forward] from here – we shouldn’t be here. We’ve made a complete mess of it from the beginning. But it’s absolutely key we put health equity at the heart of all our decisions going forward and that has practical implications. Take the furlough scheme for example – that will likely have reduced the damage as nine million people were saved from initial unemployment and it will be good for the economy in general because if these people have some income they can spend money.’
He adds: ‘The lessons from the last decade are that what we did damaged the health of the population. They stopped health improving and increased inequalities. If you want another decade where we fall further behind other countries and our inequalities deepen then go back to those policies from the 2010s – if that’s not what you want then learn from those miserable experiences.’
For Dr Watkins – who has seen the damage of austerity up close – those mistakes of the past cannot be allowed to be made again. He says: ‘There clearly has been damage to the economy but it should not be irreparable. But it will be irreparable if we go down previous paths. There are economic problems but we need to adopt the right policies to change society for the better.’
And Dr Grimbaldeston, who believes strong economic messaging tied in with health messaging is crucial, adds: ‘We must improve the health of the public and the economy – because without the economy we cannot do any of this and with good health will come a superb economy. We cannot afford to get this wrong again.’
Perhaps the greatest immediate concern is whether public health will, again, be among the major victims of the struggles of the country’s economy. This is a part of the health and care system which urgently needs massive investment and a thorough rebuild, not the ruthless treatment of further austerity.
And, those worries have become heightened for some in recent weeks after the Government announced it was to replace PHE with a specialist pandemic unit – in a move which could look like an attempt to pin blame for wider failings in the country’s pandemic response to an organisation which has coped admirably in the most testing of circumstances.
BMA council chair Chaand Nagpaul says: ‘We already have public health expertise in this country which is of the highest quality but despite the hard work of our colleagues in the last six months, substantial budget cuts and fragmentation of these services over years have hampered the response to the COVID-19 pandemic. We must absolutely not allow PHE and its staff to shoulder the blame for wider failings and Government decisions.’
It was a message echoed at the association’s annual representative meeting last month – with doctors passing a motion which said the global pandemic has demonstrated the need for a well-resourced national health protection function to meet current and future communicable disease threats.
If one thing is clear it is that the relationship between austerity and this pandemic has, to date, been a disastrous combination. For the sake of doctors, the public, the NHS and wider society, it is a relationship that must not be allowed to go on into the future.





