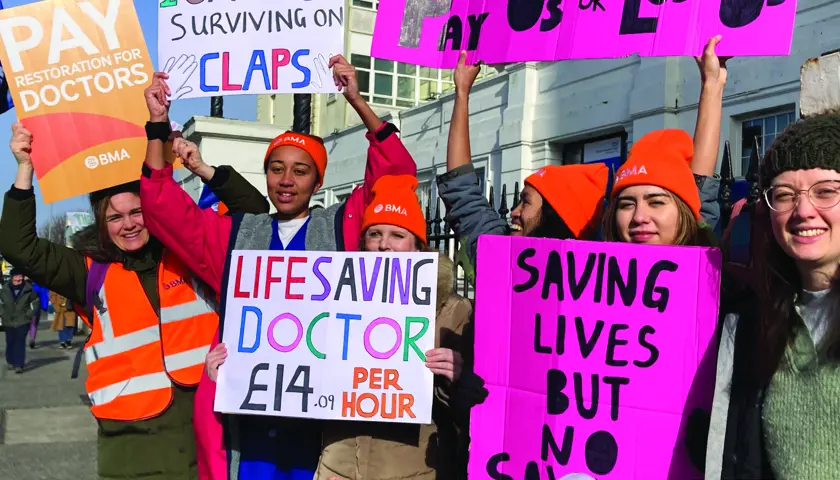
Out in force: junior doctors strike
At the start of 72 hours of planned industrial action, junior doctors sent out a clear message to the Government as they seek to restore pay to 2008 levels and improve dire working conditions. Ben Ireland and Seren Boyd joined campaigners on picket lines in London and Brighton
It’s 7am on a chilly Monday morning at The Royal London Hospital, and strong gusts of wind are blowing rubbish around the entrance to the emergency department – one of the first doctors to arrive on the picket line suggests the scene could be a metaphor for the state of NHS working conditions.
Come 7.30am, the start of the official picket, doctors kitted out in BMA high-vis jackets and beanies hold placards explaining to passers-by that junior doctors can earn as little as £14 an hour – about the same as staff at Pret A Manger, who recently received their third pay rise in 12 months.
‘I would much rather be in work today,’ says Mike Andrews, a specialty trainee 2 in internal medicine. ‘I don’t want to be here holding a placard in the cold. If [health secretary] Steve Barclay had made a meaningful offer, we’d be doing our jobs.’
Dr Andrews has seen colleagues depart, and says a recent show of hands suggested three quarters of doctors in the room would leave the NHS if strike action proves unsuccessful.
He fears: ‘If the strikes aren’t successful, we will see an exodus. It won’t be overnight, it will be slow and insidious, but this is what’s at stake. Doctors are incredibly employable, and could double our salaries working in management consulting – or move to Australia for a 50 per cent higher salary. Even medical graduates are not applying for foundation year roles, which is shocking.’
David Hobden, a respiratory ST6, notes how his pay as an foundation year 1 during the last junior doctor strikes in 2016 was only a little less than the current rate, despite living costs soaring since.
‘Doctors are feeling more and more undervalued and overworked,’ he says. ‘Five years ago, people were talking about taking a break – now people are talking about leaving.’
Louise Whitton, an ST1, changed to be a locum in order to ‘recover’ from a bruising period working through COVID during her foundation years and to give her time to apply for a training position in psychiatry.
She tells The Doctor: ‘It’s not just about our pay, it’s about making sure the hospital is staffed safely for our patients. We all feel like we’re on a sinking ship and we don’t want it to sink further. To avoid that, we need fair wages for everybody in the hospital.’
'Sinking ship'
Outside Brighton’s Royal Sussex County Hospital, passing traffic honked horns in support as about 100 doctors waved brightly coloured placards and chanted 'claps don’t pay the bills'.
Emergency department registrar Tariq Jenner says he is striking because conditions are such that he cannot give patients the treatment they deserve.
‘On a daily basis I’m treating really ill patients in corridors and in gaps between resus bays, and breaking bad news in spaces I really shouldn’t be having those conversations. We’re not treating people with dignity and that’s not acceptable. And a huge part of that is not being able to retain staff and that comes down to pay.’
Fellow striker Lara McNeill, a foundation year 3, shares Dr Jenner’s concerns about patient care.
‘So many of my colleagues are going overseas and we are so understaffed that it is risking the care of our patients,’ she says. ‘Industrial action is the only option left on the table to make the government listen.’
Many junior doctors say they are being forced to consider their options.
Hannah Baytree, a specialty trainee 4 in geriatric medicine, says: ‘I don’t want to leave being a doctor and I don’t want the situation to get any worse. But I think if things don’t change so many of my colleagues will leave that it will become unsustainable.
‘There are always rota gaps, and everyone is working short. Most people I know have either considered leaving or have an exit strategy.
‘We are not worth 26 per cent less: our work is not 26 per cent easier. If anything, it’s getting harder.
‘The government’s response is not unexpected: this government has been undermining and underfunding the NHS for a long time now, and devaluing public sector workers, not just doctors and nurses but other profession as well.’
Around 50,000 junior doctors were due to walk out across England over 72 hours from 7am on 13 March.
With inflation at budget-busting levels, NHS waiting lists at record highs and staff shortages across the board, morale has been systemically chipped away at.
Junior doctors voted overwhelmingly for industrial action in a ballot from mid-January until 20 February, with 98 per cent in favour from a 77.5 per cent turnout – an overwhelming mandate – calling on the Government to restore pay to 2008 levels.
Pay erosion
The BMA wrote to prime minister Rishi Sunak the week ahead of the action reminding him of repeated sub-inflationary pay awards which have seen junior doctors’ earnings erode by 26 per cent since 2008. Newly qualified doctors are paid as little as £14.09 an hour.
It followed a long-awaited meeting with health secretary Steve Barclay the previous week which left junior doctors committee co-chairs Rob Laurenson and Vivek Trivedi frustrated when told by Mr Barclay that he had ‘no mandate’ to negotiate on pay.
They said: ‘As tens of thousands of doctors demonstrate the strength of feeling in the profession by taking a stand through industrial action, we would remind the Government that these strikes did not have to happen if they had come to the table with meaningful proposals.
‘The cost to the Treasury to offer a fair pay deal to junior doctors that would keep more of them in the NHS and improve working conditions is negligible compared to the billions wasted on inadequate PPE and the failed test and trace system during COVID.’
Sixty per cent of the 3,000 junior doctors responding to a BMA survey in late 2022 said their morale was low or very low. Junior doctors in Scotland, who have had a 23.5 per cent real terms pay cut since 2008, are to also separately ballot for industrial action from 29 March.
Lead image credit: Andrew Baker