Cornered: GPs under attack
GPs and their practice colleagues are facing abuse, threats and violence. They tell Tim Tonkin why the Government, rather than fuelling unrealistic patient expectations about a desperately under-funded system, needs to invest in primary care and be honest with the public
The NHS’s response and role in fighting COVID-19 has, at times, seen many sections of the health service and its staff lionised by Government ministers, the public and the press.
While the merit of simply ‘clapping for carers’ could be, and has been, questioned by many in the ranks of an understaffed and under-invested-in NHS, the sentiment behind this outpouring of gratitude has not.
Yet there is another side to the national narrative on COVID and the health service, one which not only appears to be an attempt to scapegoat one part of the medical profession, but which is fuelling a disturbing rise in abuse, harassment and even violence against frontline doctors and their colleagues.
General practice, and the doctors, nurses and administrative staff who operate it, are on the receiving end of a growing tide of verbal and sometimes physical abuse from patients, apparently angered by their opposition to the vaccination roll-out, delays in accessing care owing to systemic pressures from the pandemic and claims in certain parts of the media that GPs are ‘refusing to see patients’.
'Read it aloud'
An example of abuse and intimidation, submitted to the London-wide local medical committees by a GP surgery in the capital, highlighted one of several unpleasant confrontations encountered by staff in recent weeks.
‘A patient came into reception a few weeks ago (maskless) at my practice, found no one at the front desk so barged round into the back office where staff were, shouting and pushing his phone and a letter we had sent into the face of a receptionist and repeatedly demanding she read it aloud,’ the anonymised staff member reported.
‘He was upset that we had sent him another invite for vaccination after he had specifically asked us not to. I came out to reception on hearing the commotion, along with another clinical colleague. The man was aggressive enough that we called 999 – shouting, swearing, getting very close and “squaring up” to us, despite my attempts to acknowledge our error and apologise, and offer to discuss.
‘Distressing for all concerned, as you will imagine, and this is just the worst of a number of incidents. We have had reception staff in tears several times in the last few weeks because patients or relatives have been so unpleasant.’
Primary care targeted
Another anonymous account told of how they and their colleagues had received numerous ‘abusive responses on text, via email, by phone and in person’ from patients during the pandemic.
They went on to explain that the most upsetting and unnerving instance of this abuse came when an anonymous letter warning that ‘all medical practitioners, doctors and nurses’ would be ‘on trial and held accountable for war crimes’ for their role in delivering the vaccination programme.
‘This was photocopied numerous times and put in envelopes and individually addressed to each of our clinicians and posted through the door after dark,’ the staff member noted. ‘I reported this to the police and our CCG but [got] no response from the police.’
Daily abuse
Disturbing anecdotal accounts are unfortunately all too frequently buttressed by the data drawn from multiple surveys of doctors working in primary care.
A BMA Viewpoint member survey of more than 2,400 doctors in England, Wales and Northern Ireland carried out in July, found that 46 per cent of GPs had experienced one to five incidents of verbal abuse, while roughly one-in-five (19 per cent) had received threats, in the previous month.
Within the same survey, 67 per cent of GPs said that they had witnessed violence or abuse directed at other staff in their workplace in the past year, while 37 per cent said that the instances of threatening behaviour, violence or verbal abuse they experienced had increased significantly on the same period 12 months ago.
The man was aggressive enough that we called 999 – shouting, swearing, getting very close and “squaring up” to us
Anonymised GP practice staff member
Meanwhile, a study from May this year conducted by the Institute of General Practice Management found that 75 per cent of GP staff surveyed claimed to have experienced abuse from patients on a daily basis.
‘I think every member of staff has been subject to abuse in one way or another,’ says practice manager Theresa Fielding*.
‘We have patients phoning up and shouting and swearing at them and abusing them on a daily basis. Every single member of staff has pretty much been in tears by the behaviour of patients.’
In charge of a practice in central London, Ms Fielding says that while abusive behaviour from patients was not unheard of prior to COVID, the frequency and level of abuse has definitely increased during the course of the pandemic.
She tells of how aggressive and rude behaviour is experienced across every platform the practice has for communicating with patients, from phone calls and emails, to responses to automated texts.
‘Some of the [text] responses we got back were things like “I’m going to come down there and kill you”, “I’m going to take you to the court of human rights”. We’re getting e-consultations which are littered with abuse and foul language. It’s coming at us from all angles.’
Police called
Most frightening are the occasions when patients and other members of the public attend the practice and abuse and threaten staff in person.
Ms Fielding tells of two occasions, one where she and her colleagues were confronted by a well-built, 6ft 5in tall, male patient who became aggressive and threw something at staff over the reception desk, and one where someone locked themselves into and then destroyed the practice’s toilet.
On both occasions, Ms Fielding contacted the police, but no officers attended.
‘I called the police and asked them to come out and told them that the only people in the building were four female members of staff,’ she says.
‘They [the police] said they didn’t have the resources to send anybody out while all we could hear was stuff [inside the toilet] being smashed.’
Misleading media
As unacceptable and unfair as the rise in hostility towards general practice is, the phenomenon does not appear to have begun within a vacuum, with sections of the national press having since last year set critical and accusatory tones with regard to GPs’ role within the pandemic.
A notable recent example of this has been in a tabloid newspaper, with a campaign ostensibly to increase the number of face-to-face appointments offered in practices. But in doing so, it has come up with headlines such as ‘the great GP surrender’ and called for practices which do not offer in-person consultations to be penalised.
Contrary to the narrative circulating in sections of the national media, Ms Fielding says that many GPs are actually seeing more patients than ever before, in part because of the rise in telemedicine and e-consultations, leading to unrealistic expectations.
We’re getting e-consultations which are littered with abuse and foul language
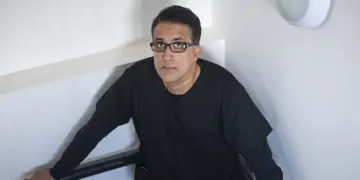
Dr Janjua
This was supported by recent NHS Digital figures for England, which showed there were 25.5 million GP appointments in August 2021, compared with 23.3 million in August 2019. ‘We have been seeing patients face-to-face but that’s not the narrative they’re getting because of what’s out in the press,’ says Ms Fielding.
‘Everybody is bashing general practice, everywhere you turn there are conversations about not being able to see a GP, or that GPs aren’t seeing patients. ‘The fact that there is this national narrative about us “not doing the job” [when] we’ve got a national shortage of GPs, we’ve got GPs off sick, we’ve got GPs with COVID who are isolating, there is no account made for that whatsoever.’
Ultimately, the effect of this climate of abuse is taking a toll on practice staff already exhausted and stretched to breaking point from COVID. ‘All of my doctors are constantly saying that they’re barely managing,’ says Ms Fielding.
‘We’ve been going into work every day to provide a service right the way through the pandemic, and yet people think it’s acceptable to swear and abuse us. ‘I know that there are staff who have had to seek support from the mental health services that are available because we can’t cope.’
Low morale
Lancashire-based GP Adam Janjua’s experience of aggressive and abusive behaviour from patients led him to make a public plea on Facebook live for general practice staff to be shown more respect.
While the video was well received by those working in healthcare, its message has not made a noticeable impact on the day-to-day realities being faced by Dr Janjua and his colleagues.
‘Barbed comments and passive aggressiveness has been on the rise ever since [the video streamed], we’re getting it daily now to be honest,’ he says.
‘GPs are fed up. They are working flat-out, 12-hour days or longer and, on top of that, having to face abuse. The least we would like is a little bit of appreciation if not from patients then at least from NHS England or the Government to say that we’re doing a good job and have carried the country through the pandemic.
‘Morale is at an all-time low and people are looking to leave [general practice] whether that means emigrating abroad or retiring early, but we are looking at a huge shortfall of staff in the next couple of years.’
Dr Janjua says he feels misinformation put out by NHS England concerning the type of services being offered by GPs, coupled with statements by the Government, had fomented an environment of suspicion and resentment towards GPs among sections of the public.
‘The trigger here I think were the NHS England press releases saying that GPs needed to start seeing patients face-to-face,’ he says. ‘That triggered a lot of anger from patients and then other people just jump on the bandwagon.’
Dr Janjua says he would like to see laws introduced that would see those guilty of physical abuse or even threats of physical abuse to NHS staff facing tougher sentences, something that the BMA has also advocated for.
He also felt that practices needed to be given powers allowing them to remove a patient from their lists if that individual had been abusive towards their staff. ‘The Government needs to change its stance and actually protect NHS staff,’ he says.
‘If you’re going to stand up and tell people or release press statements that GPs aren’t seeing patients, the retraction needs to be just as good. People will hear the scandalous stuff but if you don’t shout out that you were wrong and that general practice has always been open and is in fact operating at greater efficiency than before the pandemic, then you haven’t done enough to support general practice.’
Demand to act
Following an attack on a GP practice in Manchester on 17 September, in which four members of staff were left injured, BMA GPs committee chair Richard Vautrey held an emergency meeting with health and social care secretary Sajid Javid to urgently discuss the ‘terrible trend’ of abuse, harassment and physical attacks being levelled at general practice.
During the first of a series of planned meetings on 23 September, Dr Vautrey said the association had called on the Government to back GPs, invest in primary care and be honest with the public over pressures in the NHS.
‘This emergency meeting with the health secretary allowed us to make it crystal clear how unacceptable the increasing abuse against hardworking and dedicated GPs and the general practice workforce is.
‘We made it very clear that the Government has to explain to the public why healthcare workers are still working within the constraints of infection, protection and control measures.
‘The health secretary must confront the reality of unsustainable workload pressures, poor premises, the impact of the care backlog and secondary care work transfer to general practice. ‘Words are not enough, we now need urgent action.’
* Theresa Fielding is a pseudonym



