Don't forget us – vaccine equity around the world
Wealthy countries have reserved billions of doses of COVID vaccines while the majority of patients in poorer nations have little chance of being protected this year
For hard-pressed governments running low on public confidence and good will, the urge to buy up vast stocks of COVID vaccines for their populations is understandable.
Mass vaccination offers a much-needed boost to national morale, especially as more infectious variants of the virus emerge.
Protecting one’s own is a clear political obligation – and being seen to do so is an easy way to score points in an increasingly politicised pandemic.
But wealthy countries hoarding vaccine doses is an ugly counter to appeals for international solidarity in a global health emergency.
International bodies such as the WHO (World Health Organization) have appealed to the ethical principle of health as a universal human right and called for equitable access to vaccines.
The WMA (World Medical Association) says it is vital that ‘no country should be left behind’. Its president, David Barbe, insists: ‘We’re not just a global economy: it’s a world society now.’
This is not just a lofty moral ideal, says Julian Sheather, BMA specialist adviser in ethics and human rights.
‘If you have several billion highly impoverished people with no access to a vaccine, you have an enormous reservoir of COVID doing its Darwinian thing and it may well come back in a form that sidesteps the vaccines,’ says Dr Sheather.
Or, as the BMA puts it in a recent submission to Parliament’s foreign affairs committee, ‘pathogens do not respect borders’. Vaccine access is important to global health security.
Moral failure
It’s clear that ethicists’ ideals and market forces alone will not be enough to ensure COVID vaccines reach remote corners of war-torn Yemen or Syrian refugees.
The People’s Vaccine Alliance, a coalition of international charities, has predicted that at least 90 per cent of people in 67 low-income countries stand little chance of a COVID vaccine this year.
High-income countries, including the UK, have reserved more than half (51 per cent) of the 5.96 billion vaccine courses which manufacturers of the 13 leading COVID vaccines are projected to produce this year, according to The BMJ. And they have the option to buy more. These nations represent just 14 per cent of the global population.
Such deals prompted WHO director general Tedros Adhanom Ghebreyesus to issue a stark warning at the WHO executive board meeting in January.
The world, he said, was ‘on the brink of a catastrophic moral failure – and the price of this failure will be paid with lives and livelihoods in the world’s poorest countries’.
The price of this failure will be paid with lives and livelihoods in the world’s poorest countries
Adhanom Ghebreyesus
At that point in mid-January, 39 million doses of COVID vaccine had been given across about 49 higher-income countries. By contrast, only one lower-income nation had administered any vaccines at all. That was Guinea – where just 25 jabs had been given.
Osahon Enabulele, president of the Commonwealth Medical Association, argues that countries with under-resourced healthcare systems should have equitable access to vaccines, even if COVID case numbers are lower in such countries.
At the start of the pandemic, the Central African Republic had just three ventilators to serve the entire country, according to the International Rescue Committee; South Sudan had four. In Nigeria, where Dr Enabulele is based, healthcare workers only started receiving significant supplies of PPE (personal protective equipment) after a strike by resident junior doctors in June.
At the time of writing, COVID cases were rising again in Nigeria, the most populous African nation. ‘Public health information dissemination and risk communication mechanisms remain poor,’ says Dr Enabulele. ‘Few people are wearing masks and a lot more seem to doubt the reality of COVID-19.
‘Access to COVID-19 vaccines has nothing to do with the case numbers: it has everything to do with providing equitable access to vaccines and delivering quality care to every citizen of the world,’ Dr Enabulele says. ‘And, of course, with globalisation, even small numbers can infect the entire global community.’
Urged to share
One expression of a more equitable, internationalist approach to vaccine allocation is the COVAX Facility.
Co-led by Gavi (the Vaccine Alliance), CEPI (the Coalition for Epidemic Preparedness Innovations) and WHO, it enables countries to pool their buying power and negotiate prices collectively.
Crucially, rich countries involved agree to help finance access for the 92 lower-income countries who have signed up, through a so-called AMC (advanced market commitment).
At the time of writing, COVAX had signed deals to secure 1.3 billion doses (or 650 million vaccine courses) for these 92 nations. Its aim is to immunise one billion people with two billion doses – achieving ‘up to 20 per cent population coverage by the end of the year’ across all 190 countries taking part in COVAX.
Here, the UK has shown global leadership. It has helped to raise US$1bn for the COVAX AMC, through match-funding other donors, in addition to pledging £548m in UK aid.
‘More high-income countries must be encouraged to do the same,’ says Arthy Hartwell, BMA head of international and immigration.
But even generous contributors to COVAX, including the UK, have signed ‘side deals’ with pharmaceutical firms, raising concerns about reduced availability of vaccine for the shared pot.
Last month, WHO director general Dr Tedros urged them to share their own doses with COVAX to ensure that health workers and older people in lower-income countries took precedence in the vaccine queue over younger people in higher-income nations.
People not profit
Likewise, countries have also been urged to surrender vaccine stockpiles for COVAX’s ‘humanitarian buffer’, a reservoir of vaccine doses set aside for communities such as refugees. Canada has secured more than four doses per head of population.
Ms Hartwell says: ‘At the World Health Assembly last May, we applauded the commitment of global leaders to recognise COVID products, including vaccines, as global public goods, but since then we’ve witnessed an insidious rise in vaccine nationalism and self-interest. We must remember we are only as strong as our weakest.’
Extraordinary times demand extraordinary measures. Many believe that more should be done to ensure that vaccines should be for ‘people not profit’. Big pharma too should play its part in ensuring global access, instead of prioritising deals and regulatory approval in countries which can afford to pay.
The BMA is concerned about pharmaceuticals retaining exclusive intellectual property rights over scientific breakthroughs funded by public money. By December, AstraZeneca-Oxford, Moderna and Pfizer-BioNTech alone had received more than £3.79bn of public funding to develop their vaccines, according to People’s Vaccine Alliance estimates.
We’ve witnessed an insidious rise in vaccine nationalism and self-interest
Arthy Hartwell
Some vaccine developers have moved to assuage concerns with the potential for profiteering.
AstraZeneca’s partnership with the Serum Institute of India to manufacture vaccine doses is a promising example of collaboration.
Likewise, AstraZeneca/Oxford University has pledged to distribute 64 per cent of their vaccine in developing nations and has committed to providing vaccines to them at cost ‘in perpetuity’.
However, its ‘no-profit’ pledge does not extend beyond the pandemic for higher-income countries.
Civil society organisations have called for greater transparency over the terms of the supply-and-manufacture deals pharmaceutical firms are making, and over vaccine development and clinical trial costs.
Such information is vital if purchasers are to be able to demand fair prices in the longer term, says MSF (Médecins sans Frontières). Current vaccine prices vary wildly, from £4.40 to £54.50 per course.
Dr Sheather of the BMA argues for a less squeamish approach to pharmaceutical firms’ profits. Investing even billions of pounds of public funding in vaccine development to end a pandemic which cost the global economy an estimated £5tn last year makes good financial sense, he argues.
‘In my view, we need to look at ways in which we can accept that big pharma will get a reasonable return on its investment but, if they’re taking public funds, they must make commitments to enabling access to much less expensive vaccines in the global south as a consequence of their freedom to sell it in highly resourced markets.’
Other issues being hotly debated include whether a vaccine’s approval by the regulatory authority in one nation could suffice for countries with similar standards. Russia and China’s vaccine rollout last year under ‘emergency use authorisation’ – without data from phase 3 clinical trials – caused widespread criticism.
Distribution issues
Securing vaccines on home soil is far from the end of the story.
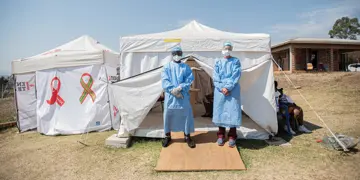
In Nigeria, Dr Enabulele says, areas beset by militant and extremist violence are virtually ‘cut off from public health interventions’: healthcare workers have been attacked, even killed, during the pandemic.
A lack of power infrastructure and appropriate cold-chain storage facilities makes distribution of mRNA vaccines such as the Pfizer/BioNTech one hugely problematic. Vaccine hesitancy, a global health threat, is a significant issue in Nigeria too.
Yet, Dr Enabulele is determinedly optimistic. COVID, he says, presents an opportunity that his country must seize.
‘Before COVID-19, people in political office would travel abroad for their care needs,’ he says. ‘But when international borders got closed as a result of the pandemic, they had no choice but to use local health facilities.
‘So, COVID-19 has engendered some greater political commitment to health. If we can maintain this momentum and disposition, I’m optimistic we can overcome COVID-19 and other healthcare challenges.’
This is not the first pandemic; it won’t be the last
Dr Barbe
Dr Barbe of the WMA predicts that some lower-income nations may require support from NGOs such as national Red Cross and Red Crescent societies. Countries at the vanguard of vaccine roll-out must share their learning on how models and strategies are having to be adapted on the ground, says Ms Hartwell.
Above all, Dr Barbe insists, a truly global response requires that every nation on the planet has a plan for effective vaccine distribution – and for the future.
‘Some countries have had sort of a national plan on paper, that just sits on the shelf gathering dust,’ says Dr Barbe.
‘That is not a plan. It has to be living and breathing, updated, rehearsed and adequately funded with the necessary infrastructure in place: that’s how we stay ready.
‘We cannot be caught flat-footed again. This is not the first pandemic; it won’t be the last. Coming together is the only way we can address this effectively and rebuild global health security.’





